Today on throwback Thursday, learn how Viagra treats depression – well, you can probably guess how, but here’s a surprise: Viagra treats sexual dysfunction in women as well as men, and it we’ll show you how in this update of our very first podcast, May 13, 2019. Oh those were simpler times.
Published On: 09/29/2022
Duration: 12 minutes, 42 seconds
Referenced Article: “Treating Sexual Side Effects,” The Carlat Psychiatry Report, May 2019 Chris Aiken, MD and Kellie Newsome, PMHNP have disclosed no relevant financial or other interests in any commercial companies pertaining to this educational activity.
Kellie Newsome: Today on throwback Thursday, learn how Viagra treats depression – well, you can probably guess how, but here’s a surprise: Viagra treats sexual dysfunction in women as well as men, and it we’ll show you how in this update of our very first podcast, May 13, 2019. Oh those were simpler times.
Chris Aiken: Welcome to the Carlat Psychiatry Podcast, keeping psychiatry honest since 2003. I’m Chris Aiken, the editor in chief of the Carlat Report.
Kellie Newsome: And I’m Kellie Newsome, a psychiatric NP and a dedicated reader of every issue.
Kellie Newsome: Dr. Adam Strassberg’s mention of how SSRI’s are capable of lowering libido, more than treating actual depression which is the very reason that these medicines are prescribed to begin with, which was really astounding to me. Dr. Aiken, can you sort of share some insight into this?
Dr. Aiken: Yes. He drew that from the rather astonishing fact that only 30% of people who take an SSRI for depression actually recover fully on them. That’s what we know from the STAR-D trial and from other metanalyses of depression trials. But around 60 to 70 percent actually have sexual dysfunction on them. So, yes, statistically he’s right. These meds are more reliable at lowering sexual function than they are at treating depression.
Kellie Newsome: Those numbers are awful!
Dr. Aiken: I agree.
Kellie Newsome: Ugh. Well, it seems that we in psychiatry can’t seem to figure out if our patients are depressed because they aren’t having sex or if it’s because of taking the SSRI medications.
Dr. Aiken: Depression is caused by many things and we need to bear in mind that sexual dysfunction itself can cause depression. We know that in part from studies of men with erectile dysfunction. I’ll tell you about a few. They took men with ED who had mild depression and gave half of them Viagra and the other half a sugar pill and, lo and behold, of course the Viagra treated their ED, but it also lifted their depression.
Chris Aiken: You have to wonder – why are we replaying old podcasts? Three reasons:
- We were surprised by how much we learned when we listened to them again. Actually we were embarrassed – I mean we created them so that really shows how much we’ve forgotten. We could all use a second go at it.
- We’re gonna update them with new research – wait for that at the end.
- Our old podcasts didn’t come with any CME credits, but these relaunches will. Just click on the link in your show notes to take the CME quiz. Here’s a sneak preview:
Kellie Newsome:
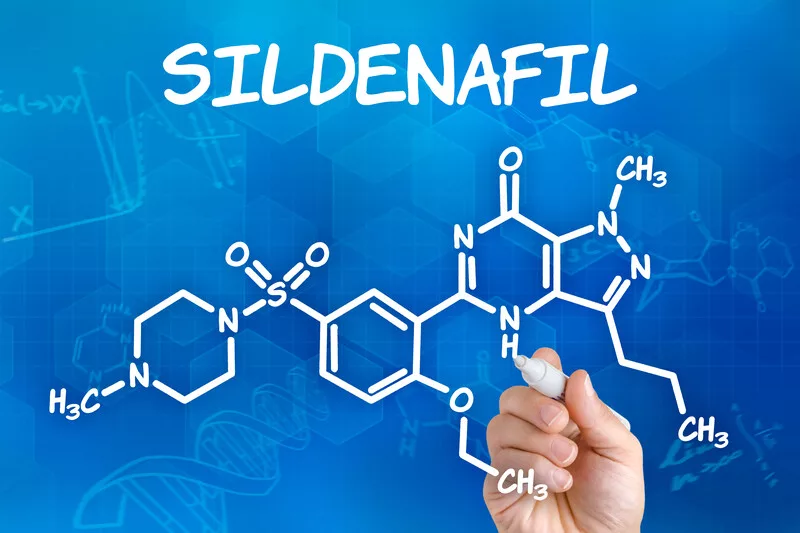
How does Sildenafil (Viagra) affect the brain?
- It blocks the serotonin 5HT2A
- It activates the serotonin 5HT2A
- It increases testosterone sensitivity
- It increases dopamine transmission in the nucleus accumbens
Kellie Newsome: Okay. So, I want to understand more about this Viagra medication, especially the part where it mentions it can work in both genders.
“And the Carlat Report slipped in a nice chart for easy reference on the medications with a low risk of side effects, as well as one with the seven antidotes for sexual dysfunction when on a serotonergic antidepressant.”
I cut mine out, personally, and I’m going to use it as a handy reference, but I want to know more.
Dr. Aiken: The way we developed that chart was simply taking everything that had at least one randomized controlled trial for sexual dysfunction. And most of the studies were done on SSRI’s. There were other studies done on antipsychotics and mood stabilizers that we touched on elsewhere. And you notice that at the top of the chart is Viagra/sildenafil both for men and women. And yes, indeed. It is the best studied antidote for sexual dysfunction on SSRI’s in both genders. I have always been surprised by that.
You know, a lot of our readers may know the study in women was a large one in the medical journal, JAMA. But it’s really hard to get women to take that. Women don’t want to bring a prescription for Viagra to the pharmacy. And one thing I learned from Dr. Strassberg’s work is these medications don’t just work by enhancing blood flow to the penis and clitoris. They actually work in the brain. Taking sildenafil increases dopamine transmission in the nucleus accumbens, also known as “the pleasure center”. So, they’re having central effects and I think that’s helpful to educate all patients, particularly women, as to why we’re giving them these medications to treat their sexual dysfunction.
Kellie Newsome: So, it seems to me like it’s such a sensitive issue, but what’s the best way? How do we ask them about their sex lives?
Dr. Aiken: Most patients aren’t going to readily bring up their sex lives in an interview, unless you’ve let that patient know that you’re comfortable hearing about it and that you’re an ally with them along the way. So, what Dr. Strassberg recommends doing is addressing it very neutrally and directly at the beginning before you prescribe the medication, warning them that this might happen and that you’ll be there to troubleshoot it with them.
And I find that to be true, too, regardless of what the symptom is, we need to create an environment where patients are comfortable talking with us about anything and they know that we’re comfortable as medical providers listening to what they have to say; that talking about their sex drive, really, to us is no different from talking about weight gain or hair loss.
Kellie Newsome: This is really helpful. I found this article totally informative on all the strategies to improve sexual dysfunction, sex lives, and all things that people can do. But I have to ask this one. At what point do we just give up and get a new partner. I mean, if all this doesn’t work, I think that has to be looked at and addressed.
Dr. Aiken: That’s a good point and it reminds me of a story I don’t often tell, but I’ll let it out here. A friend of mine is a French psychiatrist and he told me that his patients with SSRI-induced sexual dysfunction, it somehow goes away when they go out with their mistress. So, novelty can change this, but that’s not really a permanent solution, right? Because novelty wears off. But it is something that therapists for sexual dysfunction use and Dr. Strassberg talks about that, that antidotes and medications are not the only answer but often referring for couples counseling or sex therapy. And one thing they’ll do is have the couple do more novel things together, so try new activities, new experiences – both sexual and nonsexual – to stimulate that nucleus accumbens and hopefully regenerate some of that dopamine that’s being depleted, which is one of the possible pathways by which this happens.
Kellie Newsome: That actually reminds me of that term “emotional blunting”.
Dr. Aiken: Yes. Emotional blunting or apathy is another potential side effect to SSRI’s and some people speculate that it is related to sexual dysfunction. That in other words, these patients might be having apathy across the board, not just to sexual encounters. The one person who believes that is Dr. Helen Fisher. We didn’t get into this in the article, but I think it is worth mentioning. She’s a biological anthropologist and she does studies of sexual behavior.
One way she looks at that is having young adults look at pictures of the opposite sex to see how they react. And she has a study, at least one, where she was able to show that taking an SSRI blunted the reaction to just pictures. So, they might be affecting romantic behavior as well as sex itself. Specifically what she found is that the women who were put on the SSRI rated the pictures of men as less attractive and they looked at them for shorter periods of time. They just weren’t as interested. So, if a patient brings up apathy on a serotonergic agent, I would definitely wonder if their sex drive is also squashed and ask them about that.
Well, that’s all until next Monday where I hope you’ll be joining us for our second edition. We’ll be talking about a certain lap dancing drug rep who’s been making headlines lately.
Kellie Newsome: Wait! Are we going to be talking about sex again?
Dr. Aiken: No. Actually, next week we’re going to talk about money and some really disgusting things that the pharmaceutical industry has been doing recently. The lap dancing drug rep is unfortunately real, and it’s just the tip of the iceberg.
So, join us then. For now, I hope you’ll send us any …..
Chris Aiken: That was our first podcast, from May 2019, and one month later there was a big change in our understanding of sexual side effects. In June 2019, the European Medicines Agency – which is like the FDA for Europe – declared that sexual dysfunction can persist even after the antidepressant is stopped, a condition called Post-SSRI Sexual Dysfunction (PSSD). The core features of the condition are genital numbing, loss or muting of orgasm and loss of libido.
The problem was first reported in 1991, and there have been over several hundred case reports since then. Other drugs have also been implicated in persistent sexual dysfunction, like the hair loss medication finasteride and the acne treatment isotretinoin. Although the European Agency sanctioned the syndrome, it doesn’t have the gold-standard evidence of randomized controlled trials. Instead there are case studies, and lots of them. Hundreds in the literature, and another 86 just published last Spring. While it’s possible that some patients are suffering from depression or other problems that lower sex drive, in the published reports those other causes were ruled out. Likewise, these patients did not have histories of sexual dysfunction before starting the SSRI.
There is also evidence from animal studies and a possible biological mechanism supporting this syndrome. No one is sure how it happens, but it seems to be more than the old “use it or lose it” – in other words, the sex drive does not fade away from lack of use while on the SSRI. Proposed mechanisms include damage to serotonin receptors, hormonal changes, epigenetic gene expression, and dopamine-serotonin interactions.
We don’t know how common this is, but judging from the case reports it appears to be rare. How to treat it? We don’t know. But to start with, don’t invalidate your patient when they complain of it. That just makes them feel small, and later… angry at you when they google the problem and find dozens of pubmed papers on it and internet groups devoted to those who suffer from it.
Kellie Newsome: Thank you for joining us on throwback Thursdays. If you’d like to earn CME credits, follow the link in the show notes. Subscribe to the full journal with the promo code PODCAST, and follow us online where Dr. Aiken is releasing a daily dose of psychiatric research on his linked in and twitter feeds, @ChrisAikenMD.
__________
The Carlat CME Institute is accredited by the ACCME to provide continuing medical education for physicians. Carlat CME Institute maintains responsibility for this program and its content. Carlat CME Institute designates this enduring material educational activity for a maximum of one quarter (.25) AMA PRA Category 1 CreditsTM. Physicians or psychologists should claim credit commensurate only with the extent of their participation in the activity.

_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



