Crisis in Pediatric Mental Health: The Kids Aren’t Alright
CHPR: In October 2021, the American Academy of Pediatrics and the American Academy of Child and Adolescent Psychiatry both declared a national emergency in pediatric mental health. What led to that declaration, and what should hospital clinicians be aware of?
Dr. Ng: We’ve been in a silent pandemic of children’s mental health since well before the COVID-19 pandemic. Suicide is the second leading cause of death in individuals ages 10–24. One in five children have a mental health, developmental, or behavioral condition. Prior to COVID-19, we were already seeing many kids showing up in emergency departments (EDs), and COVID-19 only exacerbated the mental health crisis for kids. Rates of suicide attempts rose sharply, particularly for adolescent females (www.tinyurl.com/yc8ya9sy). Not only did kids have very disrupted lifestyles, with the loss of peer groups, opportunities to participate in sports, and rituals of graduation, but many also were not being cared for at home. One report found that about 55% of kids experienced psychological abuse at home and about 11% experienced physical abuse during the COVID-19 pandemic (Krause KH et al, MMWR Suppl 2022;71(3):28–34).
CHPR: Wow, that’s alarming. And to make things worse, many kids had been receiving mental health services in school, so with schools being closed, they were not getting any help.
Dr. Ng: Correct. We know that lower-income kids and those on Medicaid are likely to receive their mental health services within schools. So, when kids returned to school, not only had they fallen behind academically, but they were also negatively affected in their mental health and developmental needs. One study found that adolescent females in 2021 presented with more depression, eating disorders, tics, and OCD (Radhakrishnan L et al, MMWR Morb Mortal Wkly Rep 2022;71(8):319–324).
CHPR: Do you think social media contributed to these worsening mental health outcomes? And if so, what can we do to help reduce the negative impact of social media?
Dr. Ng: I think that social media is a contributing factor since 95% of youth are on some online or social media platform (www.tinyurl.com/2p9adtxw). Youth are increasingly impacted by their exposure to social media’s manipulative algorithms. Clinicians should encourage parents not only to be involved with how their youth are spending their time, but also to provide them with alternatives to social media.
CHPR: We’re seeing more kids than ever coming into EDs. Are there any new strategies to address these problems?
Dr. Ng: Yes, we’re looking at three strategies to create a larger safety net for youth. The first is to integrate collaboratively with primary care and pediatricians. Fewer than half of the families that are referred to mental health providers ever follow up. There’s a lot of stigma, but if they receive mental health services in their pediatrician’s clinic, this sidesteps some of the stigma issues. The National Network of Child Psychiatric Access Programs provides psychiatric consultation to pediatricians so they can consult a child and adolescent psychiatrist over the phone and hopefully be able to treat the child within their pediatric practice. Pediatricians and primary care providers can sign up at this website: www.nncpap.org. These child psychiatry access programs are successful and have been expanding across the country with the support of federal funding.
CHPR: Those sound like promising programs. What’s the second strategy?
Dr. Ng: The second strategy involves schools. Kids spend more time in schools than anywhere else besides their homes. We want to provide school-based mental health and to normalize schools as places where we deliver mental health care. Schools can support parents if stigma, transportation, childcare, or other barriers exist to accessing mental health care in more traditional settings, such as mental health clinics. These barriers disproportionately impact youth of color and their families. We clinicians can encourage kids and families to seek help from their school-based mental health programs wherever these programs are available.
CHPR: And the third strategy?
Dr. Ng: The third strategy is increased funding for certified community behavioral health clinics (CCBHCs). These are centers for mental health that are embedded within their communities and that often reflect the community’s language, culture, and identity. Clinicians can access the Substance Abuse and Mental Health Services Administration website to find CCBHCs in their area (www.findtreatment.samhsa.gov). According to a recent survey, 84% of these clinics already provide direct services on site at elementary, middle, and high schools or plan to in the future. Sixty-three percent of CCBHCs engage in suicide prevention programming for youth (www.tinyurl.com/2s3myjep). 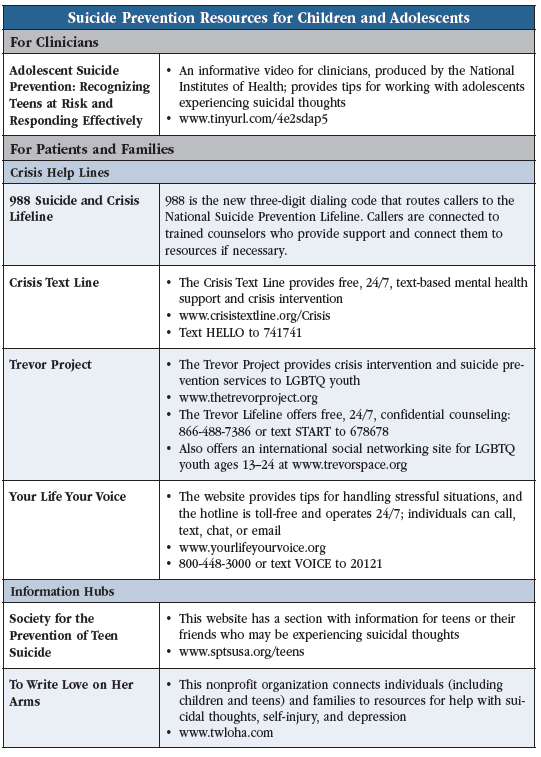
CHPR: What tips can you give us to help reduce suicidality in adolescents who show up to our EDs?
Dr. Ng: Make sure to screen for drug and alcohol use, which are strongly linked with suicidal behavior in adolescents (Wong SS et al, Soc Psychiatry Psychiatr Epidemiol 2013;48(10):1611–1620). With last summer’s introduction of 988, the national suicide hotline, there will hopefully be increased resources for childrenauto, youth, and families. I also recommend an informative National Institutes of Health video that provides tips for clinicians who work with adolescents experiencing suicidal thoughts (Editor’s note: See table). And I can’t stress enough how critical it is for adolescents to have close follow-up soon after they are discharged from EDs and inpatient psychiatry units. We can decrease suicide risk by ensuring that youth have an outpatient follow-up visit within no more than seven days of discharge (Fontanella CA et al, JAMA Netw Open 2020;3(8):e2012887). And clinicians should talk with families before discharge to address any hesitancy families may have with connecting to follow-up care—whether due to stigma, affordability, or access—so they can provide more tailored resources or information.
CHPR: Do you think we’ll get to a point where fewer kids need inpatient psychiatric beds?
Dr. Ng: I wish that all we needed to do was to put mental health into schools and primary care clinics, but given how sick some of these kids are, we still need more intensive treatment. And acute psychiatric care is only helpful if we can create a continuum of care after hospitalization and discharge to help the child maintain stability. It’s essential for us to have a more coordinated system of care and to have more child and adolescent mental health providers.
CHPR: Any final thoughts?
Dr. Ng: We are all inevitably going to see more kids in ED and inpatient psych settings, so we should be prepared for this increase and have strategies in place to mitigate future visits. The health and welfare of kids is a responsibility that falls on all of us.
CHPR: Thank you for your time, Dr. Ng.
 Warren Y.K. Ng, MD.
Warren Y.K. Ng, MD.

_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



