Do you say “antidepressant”?
“Mood stabilizer”?
Or do you tell the truth—“It’s an antipsychotic”—and watch your patient flinch?
We’ve all had this moment. The treatment fits. The label doesn’t.
Psychiatry is full of these language traps.
We use medications for reasons that don’t match their names.
Antidepressants for anxiety. Antipsychotics for mood.
And when patients ask for clarity, we give them contradiction.
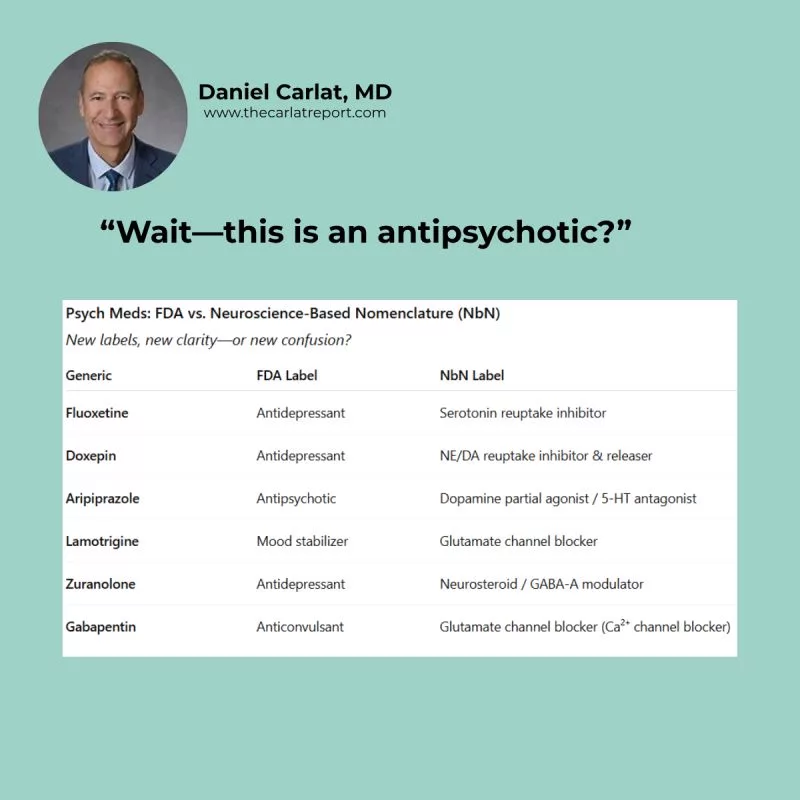
That’s why some clinicians are turning to Neuroscience-Based Nomenclature (NbN)—a system that classifies meds by mechanism instead of indication.
No more “antipsychotic.” Just: dopamine/serotonin partial agonist.
No more “antidepressant.” Just: GABA-A receptor modulator.
In theory, it’s precise. In practice, it’s a mouthful.
Is it more helpful to tell a patient they’re taking a “neurosteroid” or a “GABA modulator”?
Maybe. But maybe we’ve just swapped old stigma for new jargon.
At Carlat, we’ve been debating this ourselves—enough to write two separate pieces this year:
• TCPR: Neuroscience-Based Nomenclature: Significance to Psychiatrists
• CCPR: What is Neuroscience-Based Nomenclature?
Bottom line? NbN reframes how we talk about meds—but it doesn’t make the conversation easy. And--this is the Carlat skeptic in me--it gives prescribers a false sense of confidence that we know what we're talking about. So I’m curious:
Have you used NbN language with patients?
Did it help—or did it confuse things even more?
Join the conversation on LinkedIn with Dr. Carlat
Related Articles
- Listen to The Carlat Psychiatry Report, October 2024, Volume 22 Issue 9: “Antidepressants” Author: Gregory Malzberg, MD
- Off‑Label Strategies for Common Psychiatric Conditions Author: Chris Aiken, MD
- Philosophy of Psychiatry: Key Essentials for Therapists Interviewee: Daniel Aftab, MD

_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



