Home » Helping Clinicians Manage Teen Suicide Risk
Helping Clinicians Manage Teen Suicide Risk
January 1, 2018
From The Carlat Child Psychiatry Report
Cynthia R. Pfeffer, MD
Professor of psychiatry and director of the Childhood Bereavement Program at Weill Cornell Medicine, White Plains, NY
Dr. Pfeffer has disclosed that she has no relevant financial or other interests in any commercial companies pertaining to this educational activity.
CCPR: Thank you, Dr. Pfeffer, for participating in this interview on youth suicide. To start us off, how have clinicians come to understand risk factors for teen suicide?
Dr. Pfeffer: Historically, psychiatrists did not focus on identifying and treating risk factors for child and adolescent suicidal behavior. But after an increase in youth suicide rates in the 1980s, we started doing more research to get clarity about the issues. For example, we became aware that there were clusters of youth committing suicide—doing so in the same community and during the same time period. We suddenly recognized that hearing about a peer committing suicide would raise the risk for that peer’s close friends. This caused concern for mental health professionals and those in the community, who became interested in what factors promoted suicide among clusters of young people.
CCPR: Interesting. How different was that from how you were originally taught as a clinician?
Dr. Pfeffer: When I was in training as a child and adolescent resident, we were not taught about child and adolescent suicide. I started my research on this extensive problem when I worked to assess childhood psychiatric emergency cases. Children and their parents reported to me that children—who wanted to die—ran into traffic, attempted to jump off buildings or out of their apartment windows, overdosed, or attempted to hang themselves. People thought young children did not know about death and did not understand that it was permanent. But the issue is not whether these children understand death; it is that they want to die. We’ve come a long way since then. The National Institutes of Health (NIH), the Substance Abuse and Mental Health Services Administration (SAMHSA), and other foundations have supported research on this mental health issue and educated the community about ways to prevent youth suicide. However, it continues to be a significant problem and requires continued research for prevention.
CCPR: You mention the research that began on risk factors in the 1980s. What has the historical epidemiology on adolescent suicide looked like since then?
Dr. Pfeffer: Rates in adolescents, teens 15–18, were increasing throughout the 1980s, then decreased through about 2004. But the rates have been rising in the past 10 years, including among younger children. The causes for this are still to be determined (Ed note: The 2004 black box warning on antidepressants was associated with a drop in prescriptions and a rise in suicide rates), but suicide rates in prepubertal girls have increased significantly in the past 10 years (Curtin SC et al, MMWR Morb Mortal Wkly Rep 2017;66:816). Epidemiology statistics suggest that black American teens living in rural areas, particularly in the South, had a lower suicide rate than those in northern urban regions. A hypothesis was that black youth living in urban areas were dealing with more socioeconomic stressors. Today, while the suicide rates in the black youth population are still lower than those of white youths, they are rising. Additionally, there is evidence of increased rates of suicide among Asian American youth. This epidemiological information suggests that more work is needed to understand and prevent factors related to youth suicide.
CCPR: What is known about youth suicide risk factors?
Dr. Pfeffer: There are several broad categories of youth suicide risk factors: psychiatric disorders, family and social-related risk factors, and biological domains, including developmental, genetic, and neurodevelopmental risk factors. The most significant psychiatric risk factor for suicide or self-harm in children and adolescents is a history of suicidal behavior and ideation. Suicidal acts, especially near-lethal ones, place youth at particularly high risk for future suicide. Psychological autopsy studies point out that 90% of youth who committed suicide had a mental disorder: mostly mood disorders, especially major depression, and substance abuse (Nock MK et al, JAMA Psychiatry 2013;70(3):300). Suicidality in depression is heightened when there are psychotic features, such as in bipolar disorder with rapid cycling.
CCPR: Those are very important factors. Are there others we should be thinking about?
Dr. Pfeffer: Recently, Tourette’s disorder has been associated with increased suicide risk (Fernandez de la Cruz L, Biol Psychiatry 2016;82(2):111–118). There are high suicide rates associated with eating disorders, especially among girls, and other studies show higher rates with conduct disorder and ADHD. Youth suffering from schizophrenia are at significant risk for suicide. These conditions carry different risk levels. Another diagnostic area is autism spectrum disorder (ASD). Some children and adolescents with ASD, especially those who are high functioning, harbor suicidal thoughts and have attempted suicide. Such children and adolescents struggle with social stress and feelings of isolation and inadequacy.
CCPR: What are the family-related risk factors?
Dr. Pfeffer: Family turmoil is another big category, including acrimonious family interactions, separations and losses, and abuse. Family psychopathology is a significant factor, especially transmission of suicidal behavior through family generations. Youngsters are at higher risk when a parent is psychiatrically ill. Abuse is another significant risk factor, including physical abuse, but especially sexual abuse. It is essential to conduct a thorough family history assessment, and to gather this information systematically by asking about each close relative’s history of psychopathology. Ask parents if they have been depressed or anxious or had suicidal ideation or behavior, or other emotional problems. Specifically ask this about each close relative. Identifying these risk factors will help in treatment planning for the suicidal child or adolescent. Each family risk factor will elevate risk for suicide among youth.
CCPR: I know that bullying fits into social risk phenomena. Can you tell us more?
Dr. Pfeffer: Bullying is a more recently characterized risk factor in the US. The effect of bullying on suicide is a form of abuse by peers that happens verbally, physically, and through social media. This is observed among prepubertal children and adolescents. In the 1990s, Dr. Vincent Felitti and his colleagues studied the impact of early social stress, termed adverse childhood experiences (ACEs), and found significant impact of ACEs on development of later psychopathology and physical maladies (Felitti VJ et al, Am J Prev Med 1998;14(4):245–258).
CCPR: How is suicidal risk different in teens?
Dr. Pfeffer: Because most psychiatric disorders have adolescent onset, suicidal ideation and acts are more prevalent among adolescents. For example, bipolar disorder usually has an onset during adolescence, and it often first manifests as severe depression with intense suicidal ideation or serious suicide attempts. Adolescents have also accumulated more risk factors by that age. Furthermore, the greater developmental social independence that occurs during adolescence has many benefits and drawbacks. For example, adolescents can more successfully escape a hostile home environment. But, by leaving home, they may find themselves in new and vulnerable situations, such as school truancy, drug abuse, and exposure to sexually transmitted diseases. An important and frequent acute stress is the loss of a boyfriend or girlfriend. Another prevalent stressor is related to academic stress, which may be amplified by an unrecognized learning disability or inattention related to an anxiety disorder or attention deficit disorder.
CCPR: Are there specific risks among younger children?
Dr. Pfeffer: Prepubertal children, for better or worse, are more dependent on their parents and other relatives. When there are family problems related to parental psychopathology or other stresses on the parents, young children may be moved out of their parental home to live with relatives or foster families. Such children often suffer intense bereavement with depressive symptoms, longing for their parents, aggression, anxiety, hopelessness, and oppositional behavior. The hopelessness of losing parental nurturing may increase thoughts about dying and lead to kids planning methods to commit suicide.
CCPR: Are there other populations at risk who we haven’t mentioned yet?
Dr. Pfeffer: It is now recognized that the LGBTQ youth population is at high suicide risk, particularly for those who come out about their sexual orientation at an earlier age—by 10 or 11 for boys, or 12 or 13 for girls (Kann L et al, MMWR Surveill Summ 2016;65(9):1–202). Coming out as LGBTQ often occurs in mid-late adolescence. However, many LGBTQ teenagers may not want to come out for fear they’ll have to endure the social stressors and peer rejection. Those social stressors can lead to an increased risk for suicidal ideation or acts. Shame is a general risk factor for suicidality, which can occur when there is rejection by peers, family, and society. LGBTQ males and females require significant support from parents and school officials, and they may need psychiatric interventions to endure the long process of coming out and adjusting to being open about their sexual orientation.
CCPR: In the office setting, how should we assess suicidal risk?
Dr. Pfeffer: In the office setting, assessing suicide risk is no different than for emergency service or psychiatric inpatient settings. However, psychiatric assessment is needed, including specific questions about suicidal thinking, planning, and attempts, plus inquiry about other psychiatric, family, social, and neurobiological risk factors. It is important to recognize that younger children will minimize their understanding of risk for death. They might think one aspirin is lethal, and might not think jumping from a window will kill them. Additionally, frequency of suicidal thinking is an estimation of suicidal risk. Those with frequent suicidal ideation may be at higher risk for suicidal acts. Ask questions such as, “How many times in each hour do you think about suicide?” Ask about the amount of time spent, and how often this occurs during the day. Is it once or twice a day? New approaches to track suicidal thinking are in development, such as cell phone apps that catalog, chart, and analyze the timing, frequency, and intensity of suicidal thinking.
CCPR: That’s very helpful. Is there anything else we should know about the assessment?
Dr. Pfeffer: Clinicians need to be methodical, but not tedious in going through all the risk factors. Keep an order in mind while doing this, and use a style that is conversational; however, avoid a checklist approach, which can become stilted and let patients deny or minimize what they are thinking. More information is apparent during a discussion. Child psychiatrists need to be skilled, and this needs to be part of fellowship training with supervision. It is important for the therapist to talk very openly, and it’s best to use a stepwise approach in the type of words we use.
CCPR: This is really helpful. Can you tell us how you phrase these questions?
Dr. Pfeffer: For example, try to ask, “Do you ever think that you want to die? What did you think about?” If a child starts with the word suicide, try to understand what the child means. Do not assume the child is saying what you think is being said. We don’t really talk as much about what death means, but rather we think in terms of what the child thought about doing. Ask a child or adolescent, “Tell me more about what you were thinking. When do you have thoughts of suicide? What might help you feel better?” Pursue more specific questions about self-harm. “Did you ever think you wanted to hurt yourself? Tell me more about it. Did you ever think you wanted to do something to cause you to die? Did you ever try to do something to harm yourself or to cause you to die? Did you ever try to commit suicide? Did you think that there was something else you could do instead to feel better?”
CCPR: So, what is the next step following that assessment?
Dr. Pfeffer: It’s essential to help children or adolescents and their parents create a safety plan. This is based on the assessment. It must be relevant and meaningful and actionable, including an assured way that, if children think about acting on thoughts of self-harm, they will put themselves into a safer situation, talk with someone, and be with someone. It’s necessary to identify those helping people, but not someone who is difficult to reach. Children or adolescents need someone in proximity who is reliable, someone they are not afraid to tell about their suicidal thoughts or acts, and someone who is not afraid to help them. I have seen examples of an adolescent telling a peer, but subsequently the peer is afraid to tell a teacher or parent due to fear of creating upset or getting people in trouble. This plan should not only include peers, but also adults with whom the adolescent feels comfortable. In school, a guidance counselor or teacher may be helpful.
CCPR: How do you decide on the level of care needed for a patient to address suicidality?
Dr. Pfeffer: Prevention and intervention are guided by the assessment of risk factors. Level of care is a gradient, and you need to be familiar with what services are available in the community. All planning should include psychotherapy and consideration of treatment with medication. Outpatient care is most common. We need to work carefully on deciding how many times a week the child or adolescent will be seen, plan for work with the parents, and help the family cope. Because of expertise in assessing and treatment planning that could include use of medication, psychiatrists should be on the intervention team.
CCPR: How should we proceed if there has been a serious attempt at suicide?
Dr. Pfeffer: Because hospitalization enhances safety for an acutely suicidal child or adolescent, consider admission to a psychiatric inpatient setting. Psychiatric inpatient services are helpful in providing a comprehensive evaluation of risk factors and starting interventions such as medication, cognitive strategies, family therapy, and planning for outpatient safety strategies. Hospitalization is used to reduce suicidal ideation, symptoms of psychiatric disorders, and family conflicts, as well as to educate the child or adolescent and parents about maintaining safety and compliance with treatment. Psychiatric day hospital programs are also available in some communities. These may give relief from school stress. But because the child or adolescent goes home at the end of the day, it may expose the child or adolescent to situations that could precipitate suicidal ideation or acts. It is essential to have an effective safety plan for children or adolescents treated in less restrictive settings than a psychiatric inpatient hospital.
CCPR: Are there some resources we should be recommending to parents?
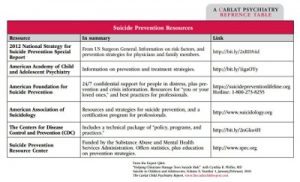
Dr. Pfeffer: There are several resources for families, including the American Academy of Child and Adolescent Psychiatry, American Foundation for Suicide Prevention, and American Association of Suicidality. (See Suicide Prevention Resources table above)
CCPR: Thank you for your time, Dr. Pfeffer.
Child PsychiatryDr. Pfeffer: Historically, psychiatrists did not focus on identifying and treating risk factors for child and adolescent suicidal behavior. But after an increase in youth suicide rates in the 1980s, we started doing more research to get clarity about the issues. For example, we became aware that there were clusters of youth committing suicide—doing so in the same community and during the same time period. We suddenly recognized that hearing about a peer committing suicide would raise the risk for that peer’s close friends. This caused concern for mental health professionals and those in the community, who became interested in what factors promoted suicide among clusters of young people.
CCPR: Interesting. How different was that from how you were originally taught as a clinician?
Dr. Pfeffer: When I was in training as a child and adolescent resident, we were not taught about child and adolescent suicide. I started my research on this extensive problem when I worked to assess childhood psychiatric emergency cases. Children and their parents reported to me that children—who wanted to die—ran into traffic, attempted to jump off buildings or out of their apartment windows, overdosed, or attempted to hang themselves. People thought young children did not know about death and did not understand that it was permanent. But the issue is not whether these children understand death; it is that they want to die. We’ve come a long way since then. The National Institutes of Health (NIH), the Substance Abuse and Mental Health Services Administration (SAMHSA), and other foundations have supported research on this mental health issue and educated the community about ways to prevent youth suicide. However, it continues to be a significant problem and requires continued research for prevention.
CCPR: You mention the research that began on risk factors in the 1980s. What has the historical epidemiology on adolescent suicide looked like since then?
Dr. Pfeffer: Rates in adolescents, teens 15–18, were increasing throughout the 1980s, then decreased through about 2004. But the rates have been rising in the past 10 years, including among younger children. The causes for this are still to be determined (Ed note: The 2004 black box warning on antidepressants was associated with a drop in prescriptions and a rise in suicide rates), but suicide rates in prepubertal girls have increased significantly in the past 10 years (Curtin SC et al, MMWR Morb Mortal Wkly Rep 2017;66:816). Epidemiology statistics suggest that black American teens living in rural areas, particularly in the South, had a lower suicide rate than those in northern urban regions. A hypothesis was that black youth living in urban areas were dealing with more socioeconomic stressors. Today, while the suicide rates in the black youth population are still lower than those of white youths, they are rising. Additionally, there is evidence of increased rates of suicide among Asian American youth. This epidemiological information suggests that more work is needed to understand and prevent factors related to youth suicide.
CCPR: What is known about youth suicide risk factors?
Dr. Pfeffer: There are several broad categories of youth suicide risk factors: psychiatric disorders, family and social-related risk factors, and biological domains, including developmental, genetic, and neurodevelopmental risk factors. The most significant psychiatric risk factor for suicide or self-harm in children and adolescents is a history of suicidal behavior and ideation. Suicidal acts, especially near-lethal ones, place youth at particularly high risk for future suicide. Psychological autopsy studies point out that 90% of youth who committed suicide had a mental disorder: mostly mood disorders, especially major depression, and substance abuse (Nock MK et al, JAMA Psychiatry 2013;70(3):300). Suicidality in depression is heightened when there are psychotic features, such as in bipolar disorder with rapid cycling.
CCPR: Those are very important factors. Are there others we should be thinking about?
Dr. Pfeffer: Recently, Tourette’s disorder has been associated with increased suicide risk (Fernandez de la Cruz L, Biol Psychiatry 2016;82(2):111–118). There are high suicide rates associated with eating disorders, especially among girls, and other studies show higher rates with conduct disorder and ADHD. Youth suffering from schizophrenia are at significant risk for suicide. These conditions carry different risk levels. Another diagnostic area is autism spectrum disorder (ASD). Some children and adolescents with ASD, especially those who are high functioning, harbor suicidal thoughts and have attempted suicide. Such children and adolescents struggle with social stress and feelings of isolation and inadequacy.
CCPR: What are the family-related risk factors?
Dr. Pfeffer: Family turmoil is another big category, including acrimonious family interactions, separations and losses, and abuse. Family psychopathology is a significant factor, especially transmission of suicidal behavior through family generations. Youngsters are at higher risk when a parent is psychiatrically ill. Abuse is another significant risk factor, including physical abuse, but especially sexual abuse. It is essential to conduct a thorough family history assessment, and to gather this information systematically by asking about each close relative’s history of psychopathology. Ask parents if they have been depressed or anxious or had suicidal ideation or behavior, or other emotional problems. Specifically ask this about each close relative. Identifying these risk factors will help in treatment planning for the suicidal child or adolescent. Each family risk factor will elevate risk for suicide among youth.
CCPR: I know that bullying fits into social risk phenomena. Can you tell us more?
Dr. Pfeffer: Bullying is a more recently characterized risk factor in the US. The effect of bullying on suicide is a form of abuse by peers that happens verbally, physically, and through social media. This is observed among prepubertal children and adolescents. In the 1990s, Dr. Vincent Felitti and his colleagues studied the impact of early social stress, termed adverse childhood experiences (ACEs), and found significant impact of ACEs on development of later psychopathology and physical maladies (Felitti VJ et al, Am J Prev Med 1998;14(4):245–258).
CCPR: How is suicidal risk different in teens?
Dr. Pfeffer: Because most psychiatric disorders have adolescent onset, suicidal ideation and acts are more prevalent among adolescents. For example, bipolar disorder usually has an onset during adolescence, and it often first manifests as severe depression with intense suicidal ideation or serious suicide attempts. Adolescents have also accumulated more risk factors by that age. Furthermore, the greater developmental social independence that occurs during adolescence has many benefits and drawbacks. For example, adolescents can more successfully escape a hostile home environment. But, by leaving home, they may find themselves in new and vulnerable situations, such as school truancy, drug abuse, and exposure to sexually transmitted diseases. An important and frequent acute stress is the loss of a boyfriend or girlfriend. Another prevalent stressor is related to academic stress, which may be amplified by an unrecognized learning disability or inattention related to an anxiety disorder or attention deficit disorder.
CCPR: Are there specific risks among younger children?
Dr. Pfeffer: Prepubertal children, for better or worse, are more dependent on their parents and other relatives. When there are family problems related to parental psychopathology or other stresses on the parents, young children may be moved out of their parental home to live with relatives or foster families. Such children often suffer intense bereavement with depressive symptoms, longing for their parents, aggression, anxiety, hopelessness, and oppositional behavior. The hopelessness of losing parental nurturing may increase thoughts about dying and lead to kids planning methods to commit suicide.
CCPR: Are there other populations at risk who we haven’t mentioned yet?
Dr. Pfeffer: It is now recognized that the LGBTQ youth population is at high suicide risk, particularly for those who come out about their sexual orientation at an earlier age—by 10 or 11 for boys, or 12 or 13 for girls (Kann L et al, MMWR Surveill Summ 2016;65(9):1–202). Coming out as LGBTQ often occurs in mid-late adolescence. However, many LGBTQ teenagers may not want to come out for fear they’ll have to endure the social stressors and peer rejection. Those social stressors can lead to an increased risk for suicidal ideation or acts. Shame is a general risk factor for suicidality, which can occur when there is rejection by peers, family, and society. LGBTQ males and females require significant support from parents and school officials, and they may need psychiatric interventions to endure the long process of coming out and adjusting to being open about their sexual orientation.
CCPR: In the office setting, how should we assess suicidal risk?
Dr. Pfeffer: In the office setting, assessing suicide risk is no different than for emergency service or psychiatric inpatient settings. However, psychiatric assessment is needed, including specific questions about suicidal thinking, planning, and attempts, plus inquiry about other psychiatric, family, social, and neurobiological risk factors. It is important to recognize that younger children will minimize their understanding of risk for death. They might think one aspirin is lethal, and might not think jumping from a window will kill them. Additionally, frequency of suicidal thinking is an estimation of suicidal risk. Those with frequent suicidal ideation may be at higher risk for suicidal acts. Ask questions such as, “How many times in each hour do you think about suicide?” Ask about the amount of time spent, and how often this occurs during the day. Is it once or twice a day? New approaches to track suicidal thinking are in development, such as cell phone apps that catalog, chart, and analyze the timing, frequency, and intensity of suicidal thinking.
CCPR: That’s very helpful. Is there anything else we should know about the assessment?
Dr. Pfeffer: Clinicians need to be methodical, but not tedious in going through all the risk factors. Keep an order in mind while doing this, and use a style that is conversational; however, avoid a checklist approach, which can become stilted and let patients deny or minimize what they are thinking. More information is apparent during a discussion. Child psychiatrists need to be skilled, and this needs to be part of fellowship training with supervision. It is important for the therapist to talk very openly, and it’s best to use a stepwise approach in the type of words we use.
CCPR: This is really helpful. Can you tell us how you phrase these questions?
Dr. Pfeffer: For example, try to ask, “Do you ever think that you want to die? What did you think about?” If a child starts with the word suicide, try to understand what the child means. Do not assume the child is saying what you think is being said. We don’t really talk as much about what death means, but rather we think in terms of what the child thought about doing. Ask a child or adolescent, “Tell me more about what you were thinking. When do you have thoughts of suicide? What might help you feel better?” Pursue more specific questions about self-harm. “Did you ever think you wanted to hurt yourself? Tell me more about it. Did you ever think you wanted to do something to cause you to die? Did you ever try to do something to harm yourself or to cause you to die? Did you ever try to commit suicide? Did you think that there was something else you could do instead to feel better?”
CCPR: So, what is the next step following that assessment?
Dr. Pfeffer: It’s essential to help children or adolescents and their parents create a safety plan. This is based on the assessment. It must be relevant and meaningful and actionable, including an assured way that, if children think about acting on thoughts of self-harm, they will put themselves into a safer situation, talk with someone, and be with someone. It’s necessary to identify those helping people, but not someone who is difficult to reach. Children or adolescents need someone in proximity who is reliable, someone they are not afraid to tell about their suicidal thoughts or acts, and someone who is not afraid to help them. I have seen examples of an adolescent telling a peer, but subsequently the peer is afraid to tell a teacher or parent due to fear of creating upset or getting people in trouble. This plan should not only include peers, but also adults with whom the adolescent feels comfortable. In school, a guidance counselor or teacher may be helpful.
CCPR: How do you decide on the level of care needed for a patient to address suicidality?
Dr. Pfeffer: Prevention and intervention are guided by the assessment of risk factors. Level of care is a gradient, and you need to be familiar with what services are available in the community. All planning should include psychotherapy and consideration of treatment with medication. Outpatient care is most common. We need to work carefully on deciding how many times a week the child or adolescent will be seen, plan for work with the parents, and help the family cope. Because of expertise in assessing and treatment planning that could include use of medication, psychiatrists should be on the intervention team.
CCPR: How should we proceed if there has been a serious attempt at suicide?
Dr. Pfeffer: Because hospitalization enhances safety for an acutely suicidal child or adolescent, consider admission to a psychiatric inpatient setting. Psychiatric inpatient services are helpful in providing a comprehensive evaluation of risk factors and starting interventions such as medication, cognitive strategies, family therapy, and planning for outpatient safety strategies. Hospitalization is used to reduce suicidal ideation, symptoms of psychiatric disorders, and family conflicts, as well as to educate the child or adolescent and parents about maintaining safety and compliance with treatment. Psychiatric day hospital programs are also available in some communities. These may give relief from school stress. But because the child or adolescent goes home at the end of the day, it may expose the child or adolescent to situations that could precipitate suicidal ideation or acts. It is essential to have an effective safety plan for children or adolescents treated in less restrictive settings than a psychiatric inpatient hospital.
CCPR: Are there some resources we should be recommending to parents?
Dr. Pfeffer: There are several resources for families, including the American Academy of Child and Adolescent Psychiatry, American Foundation for Suicide Prevention, and American Association of Suicidality. (See Suicide Prevention Resources table above)
CCPR: Thank you for your time, Dr. Pfeffer.
KEYWORDS child_psychiatry practice_tools_and_tips
Issue Date: January 1, 2018
Table Of Contents
Recommended
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2025 Carlat Publishing, LLC and Affiliates, All Rights Reserved.

_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.jpg?1729528747)



