Home » Outpatient Psychiatric Care for Developmental Disabilities
Outpatient Psychiatric Care for Developmental Disabilities
June 1, 2013
From The Carlat Psychiatry Report
Josh Feder, MD
Director of research, Interdisciplinary Council on Developmental and Learning Disorders
Dr. Feder has disclosed that he received a small payment from Pfizer for psychopharmacology research in 2012. He is the medical director of Symplay, LLC, family games for autism. Dr. Balt has reviewed this article and found no evidence of bias in this educational activity.
Between 1.5% to 2.5% of people in the US population have a developmental disorder, which includes autism spectrum disorder (ASD) and intellectual disability (often defined by having an IQ ?70) (Morstad, D; Bethesda Institute How Prevalent Are Intellectual and Developmental Disabilities in the United States? March 2012: http://bit.ly/16omOPA).
ASD occurs in one out of 50 school children and at least 1% of older adults (Blumberg SJ et al, National Center for Health Statistics. National Health Statistics Reports. March 20, 2013; http://1.usa.gov/YFiEZW). About one third of people with developmental challenges have other mental health difficulties, and these patients are often referred to general outpatient psychiatric services for assessment and management.
The psychiatric assessment of patients with developmental challenges addresses typical symptoms found in other psychiatric conditions, although assessment may require more time and collateral information from caregivers to uncover symptoms. And while mental illness may develop de novo in this population, developmental challenges frequently contribute to, or serve as the primary basis for, psychiatric conditions.
A Basic Framework For Assessment
Here are some clinical practice guidelines based on the Floortime model for assessing a person with ASD or other developmental disability (http://bit.ly/12HzmNn).
Taking a look at relating, communicating, and problem solving makes psychiatric treatment goals more clear. Consider the patient’s ability to:
A key factor in working with the patient with developmental challenges is the caregiver’s ability to read and respond to the patient. Changes in caregiving are often associated with reactions of loss or misunderstanding, as well as anxiety, agitation, and depression. Providing support to caregivers is an essential part of treatment.
Tips for Use of Medication
While psychosocial approaches are central to good care, medication may help these efforts succeed. Typically, medications are aimed at symptoms; as with children and the elderly, start low, go slow, and recognize that treatment may require unusually low or high dosages. Try not to change more than one medication as a time and work with caregivers to give changes enough time to see whether there is benefit. Since polypharmacy is often the source of difficulty, think about how to minimize medications. SSRIs may produce more behavioral activation in persons with developmental challenges, and are less reliable for compulsive behaviors. Neuroleptics carry a higher risk of tardive dyskinesia in this population. The hazards of benzodiazepines include disinhibition, addiction, poorer memory and learning, and poorer motor control. Seizure risk is higher as well and may require caution, especially with antidepressants and neuroleptics. Many people in this population are on anti-epileptic drugs (AEDs). Blood draws are often difficult and limit the use of some medications.
Agitation
Thoughtful assessment of agitation is key to addressing the problem. Triggers may include over-sensitivity, eg, to sounds or touch, or hyposensitivity resulting in conflict when the person does not respond and caregivers become frustrated. Comprehension may be limited, with concrete misperceptions of situations. Medical problems may cause pain that the person is unable to talk about. Medical or dental procedures may be associated with painful memories. People with developmental challenges frequently have rigid routines that help them manage their world that create distress when changed. Changes in caregiving may bring sadness and anxiety, and may happen when new staff do not understand the wishes of the person or their needs for support (Charlot L & Shedlack K, NADD Bulletin 2002;5(4):1).
Aging parents may become less patient or impaired themselves, leading to dangerous patterns of interaction.
Mindfulness approaches may help caregivers reduce aggression (Singh NN et al, Res Devel Disabilities 2006;5:545–558). Agitation can be proactively avoided or managed with simple principles in the clinic, at home, or in vocational placement settings, reducing the need for medication:
(Rady Children’s Hospital San Diego, ode Grey Guidelines 2013, personal communication)
General Medical Care
Poor medical care in this population is common and associated with shorter lifespan. Primary care providers may be uncomfortable with these patients or have little time for them. As with all psychiatric patients, we must advocate for developmentally disabled patients and their caregivers. For persons with Down’s syndrome, cardiac conditions are common, as is early dementia. For persons with ASDs, it is not uncommon to be agitated by florescent lighting but not react to a broken bone (Bruder MB et al, Autism Devel Disord 2012;42(11):2498–2504).
These adults are often mistreated, led astray, and unable to make financial or medical decisions. Adult Protective Services, conservatorships, and other mechanisms are invaluable for these patients. While these mechanisms are often in place for the severely handicapped, people with less obvious developmental disabilities are often left to their own devices but may be unable to protect themselves. Common situations include signing contracts for credit cards, joining the military services, or being brought into criminal activity, cults, or other confining situations or occupations such as living with and working for people without reasonable pay or accommodations. When a problem occurs that brings the person to clinical attention, we have an opportunity to identify the circumstances and bring in social services to investigate and intervene as needed.
TCPR’s Verdict: Think through the bigger picture with people who have mental health symptoms and developmental challenges. Judicious use of medication may help a good overall plan work better, but cannot make up for an inadequate plan or misunderstood symptoms.
General PsychiatryASD occurs in one out of 50 school children and at least 1% of older adults (Blumberg SJ et al, National Center for Health Statistics. National Health Statistics Reports. March 20, 2013; http://1.usa.gov/YFiEZW). About one third of people with developmental challenges have other mental health difficulties, and these patients are often referred to general outpatient psychiatric services for assessment and management.
The psychiatric assessment of patients with developmental challenges addresses typical symptoms found in other psychiatric conditions, although assessment may require more time and collateral information from caregivers to uncover symptoms. And while mental illness may develop de novo in this population, developmental challenges frequently contribute to, or serve as the primary basis for, psychiatric conditions.
A Basic Framework For Assessment
Here are some clinical practice guidelines based on the Floortime model for assessing a person with ASD or other developmental disability (http://bit.ly/12HzmNn).
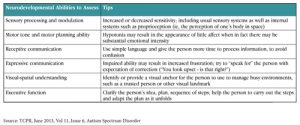
- Get a sense of the person’s experience of sensory modulation and processing. He may have difficulties with motor planning and impulsivity, as well as the comprehension of language or non-verbal cues. For example, he may have a very concrete understanding of what is said, leading him to sometimes misinterpret others, while also having difficulty reading facial expressions or tone of voice.
- Trouble with expressive communication is nearly universal, and the inadequate expression of frustration may lead to sudden reactivity.
- People with developmental challenges also often have problems with their visuospatial understanding of the world, leading to difficulties not only with field sports and classroom learning, but also everyday management of environmental settings, such as navigating stores or cafeterias.
- Limitations in cognitive and executive capacities interfere with the continuing requirements of social problem-solving, including the ability to plan, sequence, execute behaviors, and adapt to the inevitable reality that nothing ever happens quite as expected.
Functional Developmental Levels
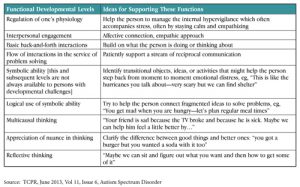
Taking a look at relating, communicating, and problem solving makes psychiatric treatment goals more clear. Consider the patient’s ability to:
- Regulate her emotions
- Connect affectively with others
- Participate in meaningful back-and-forth interaction (eg, simple responses like understanding a gesture to step up on a scale)
- Engage in a flow of interaction to solve problems (eg, negotiating where to go for a snack after an appointment)
- Use symbolic thinking for everyday challenges (eg, using a transitional object to manage separation from a caregiver)
- Employ affective ideas in social problem solving (eg, coming up with a solution to help another person feel better);
- Use higher-level reflective capacities.
Caregiver Assessment
A key factor in working with the patient with developmental challenges is the caregiver’s ability to read and respond to the patient. Changes in caregiving are often associated with reactions of loss or misunderstanding, as well as anxiety, agitation, and depression. Providing support to caregivers is an essential part of treatment.
Tips for Use of Medication
While psychosocial approaches are central to good care, medication may help these efforts succeed. Typically, medications are aimed at symptoms; as with children and the elderly, start low, go slow, and recognize that treatment may require unusually low or high dosages. Try not to change more than one medication as a time and work with caregivers to give changes enough time to see whether there is benefit. Since polypharmacy is often the source of difficulty, think about how to minimize medications. SSRIs may produce more behavioral activation in persons with developmental challenges, and are less reliable for compulsive behaviors. Neuroleptics carry a higher risk of tardive dyskinesia in this population. The hazards of benzodiazepines include disinhibition, addiction, poorer memory and learning, and poorer motor control. Seizure risk is higher as well and may require caution, especially with antidepressants and neuroleptics. Many people in this population are on anti-epileptic drugs (AEDs). Blood draws are often difficult and limit the use of some medications.
Agitation
Thoughtful assessment of agitation is key to addressing the problem. Triggers may include over-sensitivity, eg, to sounds or touch, or hyposensitivity resulting in conflict when the person does not respond and caregivers become frustrated. Comprehension may be limited, with concrete misperceptions of situations. Medical problems may cause pain that the person is unable to talk about. Medical or dental procedures may be associated with painful memories. People with developmental challenges frequently have rigid routines that help them manage their world that create distress when changed. Changes in caregiving may bring sadness and anxiety, and may happen when new staff do not understand the wishes of the person or their needs for support (Charlot L & Shedlack K, NADD Bulletin 2002;5(4):1).
Aging parents may become less patient or impaired themselves, leading to dangerous patterns of interaction.
Mindfulness approaches may help caregivers reduce aggression (Singh NN et al, Res Devel Disabilities 2006;5:545–558). Agitation can be proactively avoided or managed with simple principles in the clinic, at home, or in vocational placement settings, reducing the need for medication:
- Use simple language
- Give one-step directions when possible
- Allow time for processing questions or instructions
- Use visual schedules, either pictures or written
- Provide a “two-minute” warning prior to changes or transitions
- Provide frequent positive rewards
- Incorporate preferred or familiar items or activities
- Use visually interesting distractions during procedures (eg, bubbles)
- Allow opportunities for movement (walks, jumping, etc)
(Rady Children’s Hospital San Diego, ode Grey Guidelines 2013, personal communication)
General Medical Care
Poor medical care in this population is common and associated with shorter lifespan. Primary care providers may be uncomfortable with these patients or have little time for them. As with all psychiatric patients, we must advocate for developmentally disabled patients and their caregivers. For persons with Down’s syndrome, cardiac conditions are common, as is early dementia. For persons with ASDs, it is not uncommon to be agitated by florescent lighting but not react to a broken bone (Bruder MB et al, Autism Devel Disord 2012;42(11):2498–2504).
These adults are often mistreated, led astray, and unable to make financial or medical decisions. Adult Protective Services, conservatorships, and other mechanisms are invaluable for these patients. While these mechanisms are often in place for the severely handicapped, people with less obvious developmental disabilities are often left to their own devices but may be unable to protect themselves. Common situations include signing contracts for credit cards, joining the military services, or being brought into criminal activity, cults, or other confining situations or occupations such as living with and working for people without reasonable pay or accommodations. When a problem occurs that brings the person to clinical attention, we have an opportunity to identify the circumstances and bring in social services to investigate and intervene as needed.
TCPR’s Verdict: Think through the bigger picture with people who have mental health symptoms and developmental challenges. Judicious use of medication may help a good overall plan work better, but cannot make up for an inadequate plan or misunderstood symptoms.
KEYWORDS autism-spectrum-disorder

Issue Date: June 1, 2013
Table Of Contents
Recommended
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2026 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



