Home » Finally, Effective Treatments for Tardive Dyskinesia
Finally, Effective Treatments for Tardive Dyskinesia
May 21, 2021
From The Carlat Hospital Psychiatry Report
Farah Khorassani, PharmD.
Clinical Assistant Professor of Pharmacy Practice, St. John’s University, Queens, NY.
Dr. Khorassani has disclosed no relevant financial or other interests in any commercial companies pertaining to this educational activity.
Antipsychotics, especially first-generation antipsychotics, can cause tardive dyskinesia (TD) or abnormal involuntary movements of different areas of the body. For years, we have dreaded seeing our patients develop TD because there was little we could do about these symptoms. In 2017, the FDA approved two agents to treat TD, valbenazine (Ingrezza) and deutetrabenazine (Austedo), dramatically improving management options.
Valbenazine and deutetrabenazine inhibit the vesicular monoamine transporter 2 (VMAT2), depleting serotonin, norepinephrine, and—most important for TD symptom reduction—dopamine. Another drug, tetrabenazine (Xenazine), is also a VMAT2 inhibitor and has been available for years as an approved treatment for the chorea associated with Huntington’s disease. It is available as a generic and costs about $400/month versus about $6,000/month for the two recently approved medications. So why don’t we just use tetrabenazine? Valbenazine and deutetrabenazine have longer half-lives and can be dosed once or twice daily; in comparison, tetrabenazine needs to be taken three times daily to mitigate fluctuating plasma concentrations and has an “on-off” phenomenon when doses wear off. Tetrabenazine also has not been rigorously tested for efficacy in TD.
Efficacy
According to randomized controlled trial data submitted to the FDA, in the first 6–12 weeks of treatment, valbenazine (40–80 mg/day) and deutetrabenazine (24–48 mg/day) reduced Abnormal Involuntary Movement Scale (AIMS) scores by over 3 points—about 30%—in patients with moderate to severe TD, defined as an AIMS score > 6 (Anderson KE et al, Lancet Psychiatry 2017;4(8):595–604; Hauser RA et al, Am J Psychiatry 2017;174(5):476–484; access an online version of the AIMS asset here www.thecarlatreport.com/AIMS<Link>). Both drugs produced noticeable improvements by week 2, and patients’ symptoms lessened progressively over time, dropping by as much as 6 points over the course of 2 years (Fernandez HH et al, J Neurol Neurosurg Psychiatry 2019;90(12):1317–1323). Higher doses are more effective. For example, among patients on 80 mg/day of valbenazine, 40% showed ≥ 50% improvement at week 6, in contrast to 24% of patients on 40 mg/day.
Will patients maintain the benefit after discontinuing these drugs? Unfortunately, most patients’ symptoms return to baseline within 4 weeks of drug discontinuation, although for unclear reasons, about 1 in 6 patients do seem to maintain the response.
Side effects
Overall, valbenazine and deutetrabenazine are well tolerated, with somnolence, dry mouth, headache, akathisia, and urinary tract infections being the most common adverse effects. In clinical trials, drug discontinuation due to side effects was comparable between the active drugs and placebo (Hauser et al, 2017; Fernandez HH et al, Neurology 2017;88(21):2003–2010).
Patients receiving doses above 24 mg/day of deutetrabenazine along with other QTc-prolonging drugs should have a baseline and follow-up EKG with dose increases. Patients must also be monitored for worsening depression and suicidality, although these problems have mainly been observed in patients being treated for Huntington’s disease.
Picking a VMAT2 inhibitor
Since there are no head-to-head trials comparing the efficacy of valbenazine and deutetrabenazine, your choice of drug will depend on cost, ease of procurement, contraindications, and avoidance of drug interactions. Adverse effects are similar between both agents. Some patients might prefer the once-daily dosing of valbenazine versus the twice-daily dosing of deutetrabenazine. Both carry drug interaction potential with multiple drugs (eg, MAOIs, carbamazepine, phenytoin, St. John’s wort), so be sure to check for drug interactions before prescribing. Both drugs are expensive, and insurance policies do not always cover them, so some patients will be unable to afford these medications. You can prescribe generic tetrabenazine as an alternative, which at this point is less than a tenth the price of the two approved drugs.
Other strategies for TD management
CHPR Verdict: The VMAT2 inhibitors are game-changers in the treatment of TD, especially for patients with moderate to severe TD.
 To learn more, listen to our podcast, “Effective Treatments for Tardive Dyskinesia.” Search for “Carlat” on your podcast store.
To learn more, listen to our podcast, “Effective Treatments for Tardive Dyskinesia.” Search for “Carlat” on your podcast store.
Hospital PsychiatryValbenazine and deutetrabenazine inhibit the vesicular monoamine transporter 2 (VMAT2), depleting serotonin, norepinephrine, and—most important for TD symptom reduction—dopamine. Another drug, tetrabenazine (Xenazine), is also a VMAT2 inhibitor and has been available for years as an approved treatment for the chorea associated with Huntington’s disease. It is available as a generic and costs about $400/month versus about $6,000/month for the two recently approved medications. So why don’t we just use tetrabenazine? Valbenazine and deutetrabenazine have longer half-lives and can be dosed once or twice daily; in comparison, tetrabenazine needs to be taken three times daily to mitigate fluctuating plasma concentrations and has an “on-off” phenomenon when doses wear off. Tetrabenazine also has not been rigorously tested for efficacy in TD.
Efficacy
According to randomized controlled trial data submitted to the FDA, in the first 6–12 weeks of treatment, valbenazine (40–80 mg/day) and deutetrabenazine (24–48 mg/day) reduced Abnormal Involuntary Movement Scale (AIMS) scores by over 3 points—about 30%—in patients with moderate to severe TD, defined as an AIMS score > 6 (Anderson KE et al, Lancet Psychiatry 2017;4(8):595–604; Hauser RA et al, Am J Psychiatry 2017;174(5):476–484; access an online version of the AIMS asset here www.thecarlatreport.com/AIMS<Link>). Both drugs produced noticeable improvements by week 2, and patients’ symptoms lessened progressively over time, dropping by as much as 6 points over the course of 2 years (Fernandez HH et al, J Neurol Neurosurg Psychiatry 2019;90(12):1317–1323). Higher doses are more effective. For example, among patients on 80 mg/day of valbenazine, 40% showed ≥ 50% improvement at week 6, in contrast to 24% of patients on 40 mg/day.
Will patients maintain the benefit after discontinuing these drugs? Unfortunately, most patients’ symptoms return to baseline within 4 weeks of drug discontinuation, although for unclear reasons, about 1 in 6 patients do seem to maintain the response.
Side effects
Overall, valbenazine and deutetrabenazine are well tolerated, with somnolence, dry mouth, headache, akathisia, and urinary tract infections being the most common adverse effects. In clinical trials, drug discontinuation due to side effects was comparable between the active drugs and placebo (Hauser et al, 2017; Fernandez HH et al, Neurology 2017;88(21):2003–2010).
Patients receiving doses above 24 mg/day of deutetrabenazine along with other QTc-prolonging drugs should have a baseline and follow-up EKG with dose increases. Patients must also be monitored for worsening depression and suicidality, although these problems have mainly been observed in patients being treated for Huntington’s disease.
Picking a VMAT2 inhibitor
Since there are no head-to-head trials comparing the efficacy of valbenazine and deutetrabenazine, your choice of drug will depend on cost, ease of procurement, contraindications, and avoidance of drug interactions. Adverse effects are similar between both agents. Some patients might prefer the once-daily dosing of valbenazine versus the twice-daily dosing of deutetrabenazine. Both carry drug interaction potential with multiple drugs (eg, MAOIs, carbamazepine, phenytoin, St. John’s wort), so be sure to check for drug interactions before prescribing. Both drugs are expensive, and insurance policies do not always cover them, so some patients will be unable to afford these medications. You can prescribe generic tetrabenazine as an alternative, which at this point is less than a tenth the price of the two approved drugs.
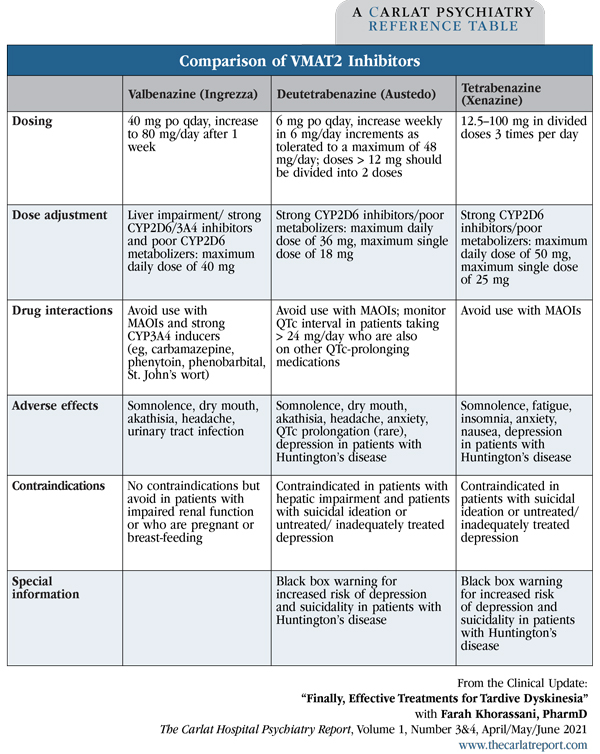
Table: Comparison of VMAT2 Inhibitors
(Click to view full-sized PDF.)
Other strategies for TD management
- If possible, switch from a first-generation to a second-generation antipsychotic. The prevalence of TD with second-generation antipsychotics is approximately 20% compared to 30% with first-generation antipsychotics (Carbon M et al, J Clin Psychiatry 2017;78(3):e264–e278).
- Lower the antipsychotic medication dose.
- Discontinue any anticholinergic drugs (eg, benztropine, trihexyphenidyl) as these may worsen symptoms.
- Consider alternative therapy with agents that also have evidence of efficacy for TD, especially when treating patients who don’t have access to VMAT2 inhibitors or for whom suicidality may be a concern. These include amantadine, vitamin B6, and vitamin E (Artukoglu BB et al, J Clin Psychiatry 2020; 81(4): 19r12798).
- Screen for TD with the AIMS every 3–6 months for all patients on any antipsychotic medication.
CHPR Verdict: The VMAT2 inhibitors are game-changers in the treatment of TD, especially for patients with moderate to severe TD.
KEYWORDS adjunct-treatment aims-test-assessment-of-involuntary-movement antipsychotics assent austedo deutetrabenazine ingrezza tardive-dyskinesia tetrabenazine valbenazine vmat2-inhibitors xenazine
Issue Date: May 21, 2021
Table Of Contents
Recommended
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2026 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



