Lithium for Children and Adolescents
Lithium is underprescribed due to clinician and family fears of side effects, and it is overutilized for off-label situations (Pérez de Mendiola X et al, Int J Bipolar Disord 2021;9(1):10). This article covers uses of lithium in children and adolescents, dosing, side effects, toxicity, and how to talk with patients and parents about lithium.
Current uses for lithium
Lithium was approved for bipolar disorder (BD) in adults in 1970 and in children 12 and older in 2018 (www.tinyurl.com/2hjhxmx6). Most research on lithium in child and adolescent psychiatry is for treating and preventing manic symptoms (McVoy M and Findling RL, eds. Clinical Manual of Child and Adolescent Psychopharmacology. 3rd ed. Washington, DC: APA Publishing; 2017). However, child psychiatrists use lithium off-label in several situations:
Major depression
Low-dose lithium augmentation is a third option for major depression alongside bupropion, T3 (Cytomel), and second-generation antipsychotics, especially after suicide attempts or co-occurring manic-like symptoms.
Mood lability
For adolescents with mood lability, dialectical behavior therapy or acceptance and commitment therapy are first line, then antidepressants, or perhaps carbamazepine or lamotrigine. If these are ineffective, consider lithium. While no medication has received FDA approval for borderline personality disorder, an older meta-analysis on lithium demonstrated benefits for irritation, anger, and self-harming behavior (Mercer D et al, J Pers Disord 2009;23(2):156–174).
Irritability
In autistic children and adolescents or in those with neurodevelopmental disorders, address functional goals and co-occurring conditions first. Then try the non-prescription and off-label options prior to trying the FDA-approved risperidone and aripiprazole (see CCPR Apr/May/Jun 2023). If none of these options work, lithium is worth trying (Mintz M and Hollenberg E, Psychopharmacol Bull 2019;49(2):28–40).
Affective aggression
For individuals with acute affective aggression and conduct disorder, the effect size of lithium (0.5) lags behind risperidone (0.72). However, lithium may be useful when risperidone is intolerable or ineffective (McVoy and Findling, 2017).
Acute psychosis
In patients with acute psychosis and comorbid affective symptoms, especially those on clozapine with its risk of agranulocytosis, lithium can target affective symptoms and possibly mitigate neutropenia (Pisano S et al, Curr Neuropharmacol 2019;17:318–341).
Anorexia nervosa
In a small case series, lithium reduced irritability in adolescent girls with anorexia nervosa (Pruccoli J et al, Riv Psichiatr 2022;57(4):198–202). We hope to see more research.
Talking with patients and caregivers about lithium
Review lithium’s risks, benefits, and alternatives with patients and caregivers. Let them know that lithium is a naturally occurring element, and that while we are still learning how it works, lithium’s mood stabilization in BD is better studied than alternatives such as second-generation antipsychotics. For off-label uses, note the limited evidence. I tell patients that side effects are usually manageable and that we will monitor benefits versus risks.
Using lithium in clinical practice
Initiating lithium
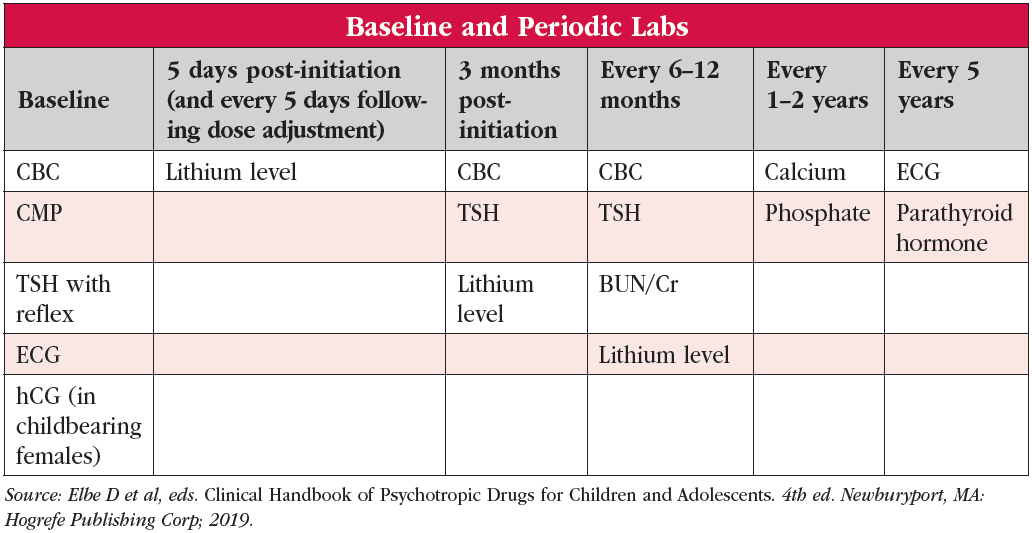
Clarify the target symptoms and severity as well as the patient’s ability to swallow medications (lithium comes in different formulations: lithium carbonate tablets and capsules, Lithobid and generic extended-release tablets, and lithium citrate oral solution). Check renal, endocrinological, neurological, cardiovascular, and pregnancy status (see “Baseline and Periodic Labs” table). Initial dosing varies based on weight and renal function. If your patient can swallow pills, extended-release lithium. This is because the adult literature demonstrates that single bedtime dosing can decrease polyuria; lead to fewer renal structural abnormalities; cause less gastrointestinal side effects, fatigue, and sedation; and allow for up to a 25% lower total dose given lithium’s lower overnight clearance (Carter L et al, Can J Psychiatry 2013;58(10):595–600; Malhi GS et al, CNS Drugs 2011;25(4):289–298).
Estimate the dose for a medium therapeutic level to reduce the number of adjustments and blood draws needed to achieve that level. In patients with normal renal function, gauge the maintenance total daily dose by weight:
- <25 kg: 600 mg/day
- 25–39 kg: 900 mg/day
- 40–50 kg: 1200 mg/day
- >50 kg: 1500 mg/day
Start at half the predicted maintenance dose. Draw a trough level five days after starting lithium and eight to 12 hours after the prior dose. The target level is 0.8–1.2 mEq/L for acute mania treatment and 0.6–1.0 mEq/L for maintenance treatment (Elbe D et al, eds. Clinical Handbook of Psychotropic Drugs for Children and Adolescents. 4th ed. Newburyport, MA: Hogrefe Publishing Corp; 2019). Adjust the dose based on lithium’s linear pharmacokinetics. If you are giving 900 mg and the level is 0.6 mEq/L, then 1200 mg should give you a level of about 0.8 mEq/L on the next level.
Maintenance treatment
Periodically monitor your patient’s lithium level and laboratory values. At each visit, review common lithium side effects:
- Gastrointestinal (eg, stomachache, nausea, vomiting, diarrhea)
- Neurological (eg, tremor, ataxia, slowed mentation, erectile difficulties)
- Renal (polyuria and polydipsia)
- Endocrinologic (weight gain, acne, cold intolerance concerning for hypothyroidism)
Common problems
Dehydration increases reabsorption of lithium, increasing lithium levels. Make sure patients hydrate, especially in hot weather, but avoid high-calorie beverages. Periodically review lithium interactions with other medications, usually related to renal clearance (McVoy and Findling, 2017):
- Non-steroidal anti-inflammatory medications (increase lithium level)
- Thiazide diuretics (increase lithium level)
- Angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers (increase lithium level)
- Theophylline and caffeine (decrease lithium level)
- Salt-repleting sports drinks (decrease lithium level)
Lithium toxicity
Lithium has a narrow therapeutic window, meaning that the level for good effect is not far below the level that might be toxic or even deadly, whether from deliberate or accidental overdose. Continuously monitor for lithium toxicity, which can include (Baird-Gunning J et al, J Intensive Care Med 2017;32(4):249–263; Elbe et al, 2019):
- Neurological (confusion, tremor, dysarthria, ataxia, nystagmus, seizures)
- Gastrointestinal (nausea, vomiting, diarrhea)
- Renal (nephrogenic diabetes insipidus, acute renal failure)
- Cardiovascular (arrhythmia, hypotension, rarely shock)
For mild toxicity (1.5–2 mEq/L), hold lithium until the level returns to target range. For moderate to severe toxicity (>2 mEq/L), use benzodiazepines for seizures along with supportive treatment—normal saline intravenous fluids and airway management. For acute ingestions, use gastrointestinal decontamination (sodium polystyrene sulfonate and/or whole bowel irrigation). Patients may require forced alkaline diuresis or hemodialysis for acute kidney failure (Baird-Gunning et al, 2017).
Discontinuing lithium
Though there are no set guidelines for discontinuing lithium, if the clinical and functional status stabilizes for six to 12 months, discuss discontinuation. Slow tapers are more successful (eg, 75% of the maintenance dose for a month, half of the maintenance dose the following month, 25% of the maintenance dose for another month, then discontinue). Continually monitor for recurrence of symptoms. Faster strategies have been employed in randomized controlled trials, such as a reduction of 300–600 mg (depending on the stable dose) weekly over four weeks until discontinued (Findling RL et al, J Am Acad Child Adolesc Pscyhiatry 2019;58(2):287–296).
CARLAT VERDICT
When used carefully, lithium is a firstline medication for BD for children ages 12 and older. Off-label situations have only limited research support, and lithium is typically third line or lower.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



