"The only thing that works for me is Xanax."
"Can I get a 3-month script for Klonopin? My last doc didn't mind."
We’ve all heard versions of these. They often trigger concern—or judgment. But behind these quotes are patients trying to manage real distress. And many of us lack a consistent, evidence-based framework beyond “use extreme caution.”
But here's the truth:
Benzos are fast, effective, and generally well-tolerated. They’re overused in some groups, underused in others. In a recent TCPR interview, Daniel Morehead, MD, laid out a smarter, more balanced way to think about them.
Here’s what we know:
- Benzos are not first-line for any anxiety disorder—but can work when other options fail
- Misuse ≠ abuse—many patients take them “off label” (e.g., during panic attacks), but not recreationally
- Young adults (15–35) are at highest risk for misuse
- Long-term users rarely escalate dose—<7% in studies
- Tapering works best when slow, collaborative, and patient-driven
- Scheduled dosing may be safer than PRN in chronic anxiety
Reframe:
We’ve moralized benzo use as if SSRIs are “real medicine” and benzos are indulgences. But anxiety has real, life-shortening risks. Shared decision-making—especially around tapering—is not just ethical, it’s clinical.
Takeaway:
Benzodiazepines aren’t villains or saviors—they’re tools. Learn which one fits the job, and work with your patients collaboratively.
Discussion Prompt:
- How do you approach benzos in patients with chronic anxiety?
- Join the conversation on LinkedIn with Dr. Carlat
- Follow for evidence-based skepticism in psychiatry
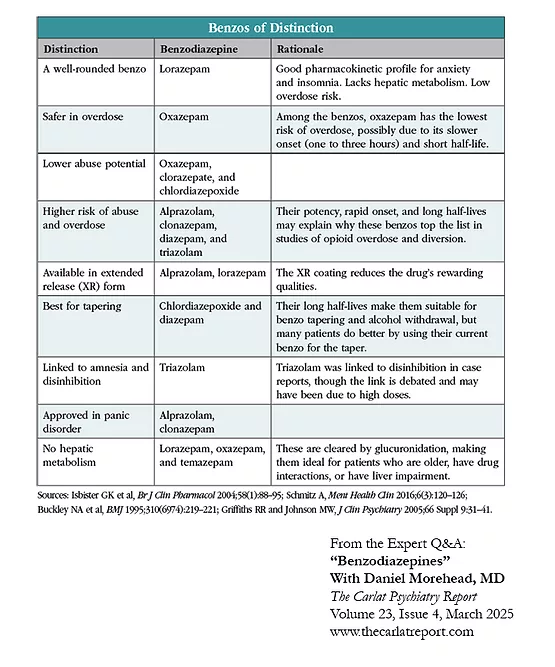
Share our "Benzos of Distinction" table with your colleagues.

Related Articles
- Benzodiazepines with Daniel Morehead, MD
- Benzodiazepines, Quetiapine, and Pregabalin for Short-Term Anxiety with Dominic Le, MD
- Psychopharm Secrets: What Patients Won’t Tell You with Chris Aiken, MD and Kellie Newsome, PMHNP
- Insomnia Treatment Update with Garrett Rossi, MD

_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



