Home » Detox: An Overview
Detox: An Overview
September 1, 2017
From The Carlat Addiction Treatment Report
 Michael Weaver, MD
Professor and medical director at the Center for Neurobehavioral Research on Addiction at the University of Texas Medical School. Author of Addiction Treatment (Carlat Publishing, 2017).
Dr. Weaver has disclosed that he received payment from Indivior in the past 12 months. Dr. Carlat has reviewed this article and has found no evidence of bias in this educational activity.
Michael Weaver, MD
Professor and medical director at the Center for Neurobehavioral Research on Addiction at the University of Texas Medical School. Author of Addiction Treatment (Carlat Publishing, 2017).
Dr. Weaver has disclosed that he received payment from Indivior in the past 12 months. Dr. Carlat has reviewed this article and has found no evidence of bias in this educational activity.
Detox (also known as “medically supervised withdrawal”) refers to treatment to help patients withdraw from substances that cause physical dependence, such as alcohol, sedative-hypnotics, and opioids. But detox is far more than a several-day process of ridding the body of an addictive substance. It should be considered an important component in the overall care and treatment of addiction.
Before beginning detox, you should ensure that your patient meets all of the following criteria:
As you begin treatment, to increase the chances of your patient achieving sobriety after detox, make sure to address the following:
The following is a substance-by-substance rundown of what you need to know when helping patients through the detox portion of their addiction treatment.
For examples of helpful 12-step substance use groups for patients, see the table below. For more information on alternative support groups to 12-step programs, see the June/July issue of CATR.
Alcohol
Withdrawal symptoms
Withdrawal symptoms begin within 24 hours of the last drink, peak at 2–3 days, and last 4–5 days on average. They include insomnia, nervousness, sweatiness, and tremors. In heavier drinkers, more serious withdrawal symptoms will begin 2–3 days after the last drink, and include more severe tremors, hallucinations, and fluctuations in pulse and blood pressure. Seizures are possible in heavy drinkers, and they tend to happen earlier in withdrawal rather than later (they may even be the presenting sign of alcohol withdrawal).
Outpatient detox
Use benzodiazepines or phenobarbital to treat alcohol withdrawal. Start with a loading dose, which is a relatively large dose that’s given every 6 hours. The purpose of this dose is to prevent withdrawal symptoms early in the withdrawal process, when those symptoms are likely to be the most severe. Consider one of the following common loading doses:
Ask the patient to hold dose if drowsy; additionally, if the patient is feeling drowsy, there should be no driving during detox. Have your patient return to see you about 24 hours after starting on the loading dose.
Although a face-to-face appointment is more effective—since it allows you to observe your patient—you can also do a phone check-in. Ask about withdrawal symptoms and look for signs of tremor, or signs of excessive sedative dose, such as drowsiness. If the loading dose has appeared effective at preventing withdrawal, give your patient a tapering dose schedule. You can simply have the patient reduce the dose by 1 pill per day, or you can write out a specific regimen. I will often specify a 5- to 10-day detox regimen, and will use a grid to make it easier for the patient to see what doses to take. (For a handy example of how to do an alcohol detox regimen, see the table below.)
Inpatient detox
Inpatient detox is similar to outpatient detox, with a tapering schedule of a sedative. The usual differences are that the detox is medically supervised by staff, and rather than giving a fixed dose, the dose is symptom-triggered, or based on the level of withdrawal symptoms. If you consider your patient to be reliable and able to follow instructions regarding the severity of symptoms requiring a sedative, outpatient detox can also be symptom-triggered.
Comfort meds
Generally, if the dose of sedative is adequate, comfort medications are not needed. However, here are some of the meds you can prescribe to treat the three primary physiological and psychiatric complaints during detox:
Opioids
For more information on commonly abused opioids, please see this table.
Withdrawal symptoms
Withdrawal symptoms peak about 12 hours after the last opiate dose and last up to 7 days. They include subjectively severe flu-like symptoms—such as nausea, aches in the lower back and legs, muscle cramps, and sometimes diarrhea; these symptoms will often progress to runny nose, watery eyes, intestinal cramps, vomiting, and muscle twitches. Instruct patients to take plenty of fluids and over-the-counter cold remedies as needed.
Outpatient detox
Tapering alone can be used in less severe cases. For example, if your patient is taking a prescribed substance such as oxycodone (eg, Percocet) and you have a clear idea of the dose that’s being taken, have the patient reduce it by half a tablet every 3–4 days. If withdrawal symptoms become too uncomfortable, have the patient slow down the reduction rate.
If you have a Drug Enforcement Administration (DEA) waiver to prescribe it, buprenorphine may be used for more severe cases. Otherwise, you can refer your patient to a physician who has a DEA waiver. Likewise, a patient can be referred to a federally licensed methadone clinic for opioid detox in an outpatient setting.
Don’t start buprenorphine treatment until after withdrawal symptoms have begun—in other words, after the patient has already experienced some nausea and muscle achiness. To do this, ask your patient to abstain from opioids for at least 24 hours before induction. Also before induction, it might be useful to measure the severity of opioid withdrawal symptoms by using the Clinical Opioid Withdrawal Scale (COWS). If the patient is not already in withdrawal, the first dose of buprenorphine could cause an even more unpleasant withdrawal experience.
Start with a dose of 2–4 mg, administered sublingually and repeated every hour or two until the patient is comfortable. Since most forms of buprenorphine have poor oral bioavailability and take at least 5 minutes to dissolve, have the patient place 1 or 2 tablets (or films) under the tongue, and then allow the medication to dissolve.
On day 2 of the induction, administer an entire day’s dose of buprenorphine at once. If necessary, go up from there, and have the patient come back to the office for additional treatment until you find the right dose. Once you’ve found it, have the patient return to the office weekly so you can make necessary dosage adjustments until the patient is abstinent.
Inpatient detox
The same strategy for switching the patient to either methadone or buprenorphine applies (including legal regulations). Here, though, the detox takes place in an inpatient environment, where there is intensive monitoring for withdrawal symptoms. After a few days in a detox facility, patients should get individual or group psychotherapy and 12-step meetings. (There are also alternatives to 12-step programs that some patients may prefer.)
Comfort meds
During tapering, you might also want to offer comfort meds, including the following:
Nicotine
Withdrawal
There are no obvious physical symptoms, but subjective ones such as reduced alertness, irritability, depressed mood, restlessness, insomnia, increased appetite, headache, and intense craving may occur. Withdrawal symptoms last 7–10 days, then drop off sharply and improve.
Smoking cessation treatment
Rather than detox, the correct term when applied to smoking might be cessation, which should include both pharmacologic and non-pharmacologic strategies.
Consider using nicotine replacement therapy (NRT), which works by supplying an alternative source of nicotine to help your patient decrease and ultimately quit smoking. Because it’s widely available and acceptable to most tobacco users, I recommend NRT before moving to bupropion (Wellbutrin) or varenicline (Chantix).
There are several NRT solutions to choose from, but consider starting with the patch, since it delivers a constant nicotine level throughout the day to prevent episodes of craving while tapering. For a 1-pack-per-day smoker, prescribe the 21 mg patch. For a 2-pack-per-day smoker, 2 patches might be needed. Many state health departments sponsor a “quit line,” through which patients who are uninsured can get the patch for free. Have your patient call 1-800-QUIT-NOW for more information.
Tell the patient to apply a new patch daily after waking up. Start by placing it just above the heart (upper anterior chest), then the next day move it to the left upper arm, then the left upper back, right shoulder, right chest, and finally back to above the heart. Have your patient stay on the initial dose for 4–6 weeks, then use the lower-strength patch for 4 weeks, and so on as the patient tapers off nicotine. Tell your patient not to smoke while on the patch, since that can cause nausea, which is the first symptom of nicotine toxicity.
For patients who continue to have cravings while using the patch, recommend that they also use nicotine gum, lozenge, or spray. For lighter smokers, you can also start by recommending nicotine gum. If patients experience insomnia or vivid dreams on the patch, suggest they remove the patch before bedtime and replace it with a new one in the morning.
If NRT is unsuccessful, varenicline (Chantix) can be tried, which acts as a partial agonist at nicotine receptors. Some patients will want to start with a pill right away instead of NRT, which is acceptable. Start varenicline 1 week before a patient’s quit date or within 8–35 days after starting it. The initial dose is 0.5 mg po daily for 3 days, 0.5 mg BID for 4 days, and then 1 mg BID thereafter. Continue at that dose for 3–6 months. You can prescribe a first-month starter kit that comes with clear instructions for how and when a patient should increase the dose. Inform patients that they may experience increased, vivid dreaming while on varenicline.
Bupropion (sustained release) is also an effective alternative. According to one large study, bupropion led to a 23% 1-year quit rate vs. 12% for placebo (Hurt, 1997). Prescribe 150 mg for 3 days, then increase to 150 mg BID as tolerated, and inform patients of the drug’s potential side effects (insomnia and anxiety).
Varenicline is likely more effective than bupropion. For example, in one trial, the 9–12 week quit rate for varenicline was 44% compared to 28% for bupropion and 18% for placebo (Nides M et al, Am J Health Behav 2008;32(6):664–675).
Two off-label meds, nortriptyline and clonidine, are worth trying. With nortriptyline, start with 25 mg per day, and increase to 75 or 100 mg daily as tolerated. Clonidine should be dosed at 0.1 mg daily, increased to a maximum of 0.75 mg daily while assessing the patient’s blood pressure.
For a table summarizing FDA-approved treatments for tobacco use disorder, see below.
Stimulants (cocaine, amphetamine, methamphetamine, designer drugs)
Withdrawal
Patients will experience fatigue, depression, irritability, increased appetite, and sometimes suicidal behavior. There is no specific treatment for stimulant withdrawal. After several days, symptoms go away and are followed by intense cravings for the specific stimulant.
Detox
There is no pharmacotherapy for stimulant addiction. Simple supportive care is most helpful, with a reassurance that the symptoms will improve over a few days. Some patients use stimulants to self-medicate an underlying depression, so if depressive symptoms persist for a week or more after the initial withdrawal phase, consider starting an antidepressant medication.
Cannabis
Withdrawal
Symptoms can include depression, irritability, anxiety, appetite suppression, and headaches. Heavy users sometimes experience diarrhea, nausea, and vomiting. Withdrawal generally lasts 3–7 days, depending on the amount of prior use, although insomnia can be more persistent. Symptoms are generally mild for most people, but they can be more severe with heavy, chronic users.
Detox
Cannabis detox is usually done in an outpatient setting. Tell your patient that the first 5–7 days of withdrawal will be difficult, and to concentrate on getting plenty of rest and fluids during that period. There are no approved medications for treating cannabis use disorder or withdrawal. Some studies imply that some medications might be effective, but more research is needed. The FDA-approved cannabinoids, dronabinol (Schedule III) and nabilone (Schedule II), may help ease withdrawal symptoms. Any practitioner can prescribe both cannabinoids, but they are expensive controlled substances, and chances are that they won’t be covered by insurance.
Comfort meds
Consider prescribing the following:
CATR Verdict: If done properly, helping addicted patients through the detox part of their recovery process can help achieve better outcomes once addiction treatment begins. It’s not just about ridding the body of addictive substances, but also about helping patients deal with withdrawal syndrome, and preparing them for the next steps toward a goal of long-term recovery.
Addiction TreatmentBefore beginning detox, you should ensure that your patient meets all of the following criteria:
- Is cognitively intact and reliable, medically and psychiatrically stable, and willing to commit to abstinence
- Has a home environment that will support sobriety
- Has, in cases of outpatient detox, safe transportation to and from the clinic
- Lacks a history of complicated withdrawal, such as seizures or delirium tremens
- Is not dually dependent on alcohol and sedative-hypnotics, alcohol and opioids, or sedative-hypnotics and opioids
As you begin treatment, to increase the chances of your patient achieving sobriety after detox, make sure to address the following:
- Understand and communicate to your patient why detox is crucial at this point in the patient’s life.
- Explain what detox will accomplish and how it will connect to ongoing treatment.
- Create a detox protocol that helps the patient come off the abused drug while experiencing as little discomfort as possible.
- Conduct a proper follow-up that offers physiological and psychopharmacological support to help the patient deal with post-acute withdrawal syndromes. Include psychotherapy and other psychosocial supports for long-term sobriety.
The following is a substance-by-substance rundown of what you need to know when helping patients through the detox portion of their addiction treatment.
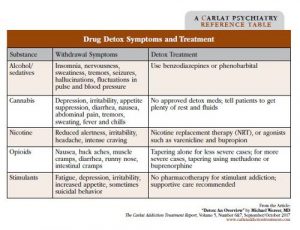
Table: Drug Detox Symptoms and Treatment
(Click here to view full-size PDF)
For examples of helpful 12-step substance use groups for patients, see the table below. For more information on alternative support groups to 12-step programs, see the June/July issue of CATR.
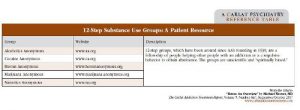
Table: 12-Step Substance Use Groups: A Patient Resource
(Click here to view full-size PDF)
Alcohol
Withdrawal symptoms
Withdrawal symptoms begin within 24 hours of the last drink, peak at 2–3 days, and last 4–5 days on average. They include insomnia, nervousness, sweatiness, and tremors. In heavier drinkers, more serious withdrawal symptoms will begin 2–3 days after the last drink, and include more severe tremors, hallucinations, and fluctuations in pulse and blood pressure. Seizures are possible in heavy drinkers, and they tend to happen earlier in withdrawal rather than later (they may even be the presenting sign of alcohol withdrawal).
Outpatient detox
Use benzodiazepines or phenobarbital to treat alcohol withdrawal. Start with a loading dose, which is a relatively large dose that’s given every 6 hours. The purpose of this dose is to prevent withdrawal symptoms early in the withdrawal process, when those symptoms are likely to be the most severe. Consider one of the following common loading doses:
- Oxazepam (Serax) 15–30 mg po q 6 hours
- Chlordiazepoxide (Librium) 25–50 mg po q 6 hours
- Diazepam (Valium) 10–20 mg po q 6 hours
- Lorazepam (Ativan) 1–2 mg po q 6 hours
- Clonazepam (Klonopin) 0.5–1 mg po q 6 hours
- Phenobarbital 15–30 mg po q 6 hours
Ask the patient to hold dose if drowsy; additionally, if the patient is feeling drowsy, there should be no driving during detox. Have your patient return to see you about 24 hours after starting on the loading dose.
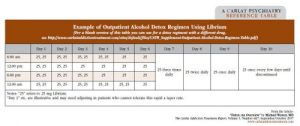
Although a face-to-face appointment is more effective—since it allows you to observe your patient—you can also do a phone check-in. Ask about withdrawal symptoms and look for signs of tremor, or signs of excessive sedative dose, such as drowsiness. If the loading dose has appeared effective at preventing withdrawal, give your patient a tapering dose schedule. You can simply have the patient reduce the dose by 1 pill per day, or you can write out a specific regimen. I will often specify a 5- to 10-day detox regimen, and will use a grid to make it easier for the patient to see what doses to take. (For a handy example of how to do an alcohol detox regimen, see the table below.)
Table: Example of Outpatient Alcohol Detox Regimen Using Librium
(Click here to view full-size PDF)
Inpatient detox
Inpatient detox is similar to outpatient detox, with a tapering schedule of a sedative. The usual differences are that the detox is medically supervised by staff, and rather than giving a fixed dose, the dose is symptom-triggered, or based on the level of withdrawal symptoms. If you consider your patient to be reliable and able to follow instructions regarding the severity of symptoms requiring a sedative, outpatient detox can also be symptom-triggered.
Comfort meds
Generally, if the dose of sedative is adequate, comfort medications are not needed. However, here are some of the meds you can prescribe to treat the three primary physiological and psychiatric complaints during detox:
- For nausea: Ondansetron 4 mg po q 8 hours prn
- For insomnia: Trazodone 50 mg qhs or diphenhydramine 50 mg qhs prn
- For anxiety: Clonidine 0.1 mg QID prn if accompanied by autonomic hyperactivity or gabapentin 150–300 mg QID prn
Opioids
For more information on commonly abused opioids, please see this table.
Table: Commonly Abused Opioids
(Click here to view full-size PDF)
Withdrawal symptoms
Withdrawal symptoms peak about 12 hours after the last opiate dose and last up to 7 days. They include subjectively severe flu-like symptoms—such as nausea, aches in the lower back and legs, muscle cramps, and sometimes diarrhea; these symptoms will often progress to runny nose, watery eyes, intestinal cramps, vomiting, and muscle twitches. Instruct patients to take plenty of fluids and over-the-counter cold remedies as needed.
Outpatient detox
Tapering alone can be used in less severe cases. For example, if your patient is taking a prescribed substance such as oxycodone (eg, Percocet) and you have a clear idea of the dose that’s being taken, have the patient reduce it by half a tablet every 3–4 days. If withdrawal symptoms become too uncomfortable, have the patient slow down the reduction rate.
If you have a Drug Enforcement Administration (DEA) waiver to prescribe it, buprenorphine may be used for more severe cases. Otherwise, you can refer your patient to a physician who has a DEA waiver. Likewise, a patient can be referred to a federally licensed methadone clinic for opioid detox in an outpatient setting.
Don’t start buprenorphine treatment until after withdrawal symptoms have begun—in other words, after the patient has already experienced some nausea and muscle achiness. To do this, ask your patient to abstain from opioids for at least 24 hours before induction. Also before induction, it might be useful to measure the severity of opioid withdrawal symptoms by using the Clinical Opioid Withdrawal Scale (COWS). If the patient is not already in withdrawal, the first dose of buprenorphine could cause an even more unpleasant withdrawal experience.
Start with a dose of 2–4 mg, administered sublingually and repeated every hour or two until the patient is comfortable. Since most forms of buprenorphine have poor oral bioavailability and take at least 5 minutes to dissolve, have the patient place 1 or 2 tablets (or films) under the tongue, and then allow the medication to dissolve.
On day 2 of the induction, administer an entire day’s dose of buprenorphine at once. If necessary, go up from there, and have the patient come back to the office for additional treatment until you find the right dose. Once you’ve found it, have the patient return to the office weekly so you can make necessary dosage adjustments until the patient is abstinent.
Inpatient detox
The same strategy for switching the patient to either methadone or buprenorphine applies (including legal regulations). Here, though, the detox takes place in an inpatient environment, where there is intensive monitoring for withdrawal symptoms. After a few days in a detox facility, patients should get individual or group psychotherapy and 12-step meetings. (There are also alternatives to 12-step programs that some patients may prefer.)
Comfort meds
During tapering, you might also want to offer comfort meds, including the following:
- For anxiety: Clonidine 0.1 mg po QID prn (monitor pulse and blood pressure)
- For insomnia: Trazodone 50–100
- mg po qhs prn sleep
- For diarrhea: Loperamide (Imodium) 2 mg po initially, then 2 mg prn diarrhea (max dose 16 mg
- per day)
- For body aches: Ibuprofen or acetaminophen
Nicotine
Withdrawal
There are no obvious physical symptoms, but subjective ones such as reduced alertness, irritability, depressed mood, restlessness, insomnia, increased appetite, headache, and intense craving may occur. Withdrawal symptoms last 7–10 days, then drop off sharply and improve.
Smoking cessation treatment
Rather than detox, the correct term when applied to smoking might be cessation, which should include both pharmacologic and non-pharmacologic strategies.
Consider using nicotine replacement therapy (NRT), which works by supplying an alternative source of nicotine to help your patient decrease and ultimately quit smoking. Because it’s widely available and acceptable to most tobacco users, I recommend NRT before moving to bupropion (Wellbutrin) or varenicline (Chantix).
There are several NRT solutions to choose from, but consider starting with the patch, since it delivers a constant nicotine level throughout the day to prevent episodes of craving while tapering. For a 1-pack-per-day smoker, prescribe the 21 mg patch. For a 2-pack-per-day smoker, 2 patches might be needed. Many state health departments sponsor a “quit line,” through which patients who are uninsured can get the patch for free. Have your patient call 1-800-QUIT-NOW for more information.
Tell the patient to apply a new patch daily after waking up. Start by placing it just above the heart (upper anterior chest), then the next day move it to the left upper arm, then the left upper back, right shoulder, right chest, and finally back to above the heart. Have your patient stay on the initial dose for 4–6 weeks, then use the lower-strength patch for 4 weeks, and so on as the patient tapers off nicotine. Tell your patient not to smoke while on the patch, since that can cause nausea, which is the first symptom of nicotine toxicity.
For patients who continue to have cravings while using the patch, recommend that they also use nicotine gum, lozenge, or spray. For lighter smokers, you can also start by recommending nicotine gum. If patients experience insomnia or vivid dreams on the patch, suggest they remove the patch before bedtime and replace it with a new one in the morning.
If NRT is unsuccessful, varenicline (Chantix) can be tried, which acts as a partial agonist at nicotine receptors. Some patients will want to start with a pill right away instead of NRT, which is acceptable. Start varenicline 1 week before a patient’s quit date or within 8–35 days after starting it. The initial dose is 0.5 mg po daily for 3 days, 0.5 mg BID for 4 days, and then 1 mg BID thereafter. Continue at that dose for 3–6 months. You can prescribe a first-month starter kit that comes with clear instructions for how and when a patient should increase the dose. Inform patients that they may experience increased, vivid dreaming while on varenicline.
Bupropion (sustained release) is also an effective alternative. According to one large study, bupropion led to a 23% 1-year quit rate vs. 12% for placebo (Hurt, 1997). Prescribe 150 mg for 3 days, then increase to 150 mg BID as tolerated, and inform patients of the drug’s potential side effects (insomnia and anxiety).
Varenicline is likely more effective than bupropion. For example, in one trial, the 9–12 week quit rate for varenicline was 44% compared to 28% for bupropion and 18% for placebo (Nides M et al, Am J Health Behav 2008;32(6):664–675).
Two off-label meds, nortriptyline and clonidine, are worth trying. With nortriptyline, start with 25 mg per day, and increase to 75 or 100 mg daily as tolerated. Clonidine should be dosed at 0.1 mg daily, increased to a maximum of 0.75 mg daily while assessing the patient’s blood pressure.
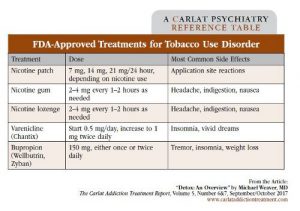
For a table summarizing FDA-approved treatments for tobacco use disorder, see below.
Table: FDA Approved Treatments for Tobacco Use Disorder
(Click here to view full-size PDF)
Stimulants (cocaine, amphetamine, methamphetamine, designer drugs)
Withdrawal
Patients will experience fatigue, depression, irritability, increased appetite, and sometimes suicidal behavior. There is no specific treatment for stimulant withdrawal. After several days, symptoms go away and are followed by intense cravings for the specific stimulant.
Detox
There is no pharmacotherapy for stimulant addiction. Simple supportive care is most helpful, with a reassurance that the symptoms will improve over a few days. Some patients use stimulants to self-medicate an underlying depression, so if depressive symptoms persist for a week or more after the initial withdrawal phase, consider starting an antidepressant medication.
Cannabis
Withdrawal
Symptoms can include depression, irritability, anxiety, appetite suppression, and headaches. Heavy users sometimes experience diarrhea, nausea, and vomiting. Withdrawal generally lasts 3–7 days, depending on the amount of prior use, although insomnia can be more persistent. Symptoms are generally mild for most people, but they can be more severe with heavy, chronic users.
Detox
Cannabis detox is usually done in an outpatient setting. Tell your patient that the first 5–7 days of withdrawal will be difficult, and to concentrate on getting plenty of rest and fluids during that period. There are no approved medications for treating cannabis use disorder or withdrawal. Some studies imply that some medications might be effective, but more research is needed. The FDA-approved cannabinoids, dronabinol (Schedule III) and nabilone (Schedule II), may help ease withdrawal symptoms. Any practitioner can prescribe both cannabinoids, but they are expensive controlled substances, and chances are that they won’t be covered by insurance.
Comfort meds
Consider prescribing the following:
- For nausea: Either promethazine (Phenergen) 25 mg po TID prn or prochlorperazine (Compazine) 5–10 mg TID prn
- For headaches: Acetaminophen or ibuprofen
CATR Verdict: If done properly, helping addicted patients through the detox part of their recovery process can help achieve better outcomes once addiction treatment begins. It’s not just about ridding the body of addictive substances, but also about helping patients deal with withdrawal syndrome, and preparing them for the next steps toward a goal of long-term recovery.

Issue Date: September 1, 2017
Recommended
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2026 Carlat Publishing, LLC and Affiliates, All Rights Reserved.



_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



