Home » Treating Pandemic-Associated Trauma in Children and Adolescents
Treating Pandemic-Associated Trauma in Children and Adolescents
March 12, 2021
From The Carlat Child Psychiatry Report
 Alan Steinberg, PhD
Associate Director of the National Center for Child Traumatic Stress at UCLA.
Alan Steinberg, PhD
Associate Director of the National Center for Child Traumatic Stress at UCLA.
 Naser Ahmadi, MD, PhD
Assistant Professor of Psychiatry at UCLA.
Dr. Steinberg and Dr. Ahmadi have disclosed that they have no relevant financial or other interests in any commercial companies pertaining to this educational activity.
Naser Ahmadi, MD, PhD
Assistant Professor of Psychiatry at UCLA.
Dr. Steinberg and Dr. Ahmadi have disclosed that they have no relevant financial or other interests in any commercial companies pertaining to this educational activity.CCPR: Tell us about your backgrounds.
Dr. Steinberg: I’m the Associate Director of the National Center for Child Traumatic Stress at UCLA.
Dr. Ahmadi: I’m Assistant Professor of Psychiatry at UCLA and Director of Family Trauma Distress at Olive View, and Dr. Steinberg and I worked together with colleagues to develop our UCLA Brief COVID-19 Screen for Child/Adolescent PTSD.
CCPR: What is the National Center for Child Traumatic Stress? What’s its purpose?
Dr. Steinberg: The problem of child traumatic stress in the US is enormous: sexual abuse, physical abuse, neglect, domestic violence, and mixtures of complex trauma histories—including kids who are exposed to natural and manmade disasters, catastrophic school violence, community violence, exploitation, trafficking, traumatic bereavement, and so on. That’s the reason for the National Child Traumatic Stress Network Initiative: to make all systems that provide care and services to children and families more trauma informed, to ask about trauma histories and PTSD, and to help these kids receive needed assessments and evidence-based interventions.
CCPR: What are some of the symptoms of pandemic-associated trauma in children? And how do you assess for these symptoms?
Dr. Ahmadi: In our current pandemic, the trauma is often related to losses and traumatic events even when the child is unlikely to have COVID. Many youths have traumatic experiences related to COVID, like having someone close to you die from COVID—a family member, schoolmate, or teacher—or having a parent working in an environment where they’re exposed to the illness or where there’s been a quarantine in the family. Our new screening instrument can help clinicians assess these concerns more specifically for better treatment planning. (Editor’s note: The UCLA Brief COVID-19 Screen for Child/Adolescent PTSD is available at no cost in both English and Spanish for use by professionals across a range of child-serving systems, including behavioral health, primary care, pediatrics, schools, child welfare, juvenile justice, and residential care. See www.tinyurl.com/uv4qu5gr.)
CCPR: Is there research specifically on the effects of COVID on mental health?
Dr. Steinberg: We know from global reports of the pandemic that many adults and children have traumatic and stress symptoms due to COVID. When you assess kids who suffer from trauma, you usually expect maybe 10% or 20% to have PTSD. In April 2020, we saw an influx of adults and children coming with much more dysregulation, and we found 20%–40% of these people had PTSD related to the pandemic, which was kind of a shock to us. This is really important because the current standard of care for trauma screening is very limited in scope.
CCPR: How do you treat children with pandemic-related PTSD?
Dr. Ahmadi: In addition to usual trauma-informed care—such as helping kids get back to familiar routines, supporting structure and new routines when that’s not possible, and supporting parents and other caregivers so they can be present and supportive and reassuring to kids—we have used two techniques that show a lot of promise. One is called “reminder-focused positive psychiatry” (RFPP) and the other is called “trauma-focused cognitive behavioral therapy” (TFCBT). RFPP is focused on helping patients identify and manage reminders of trauma that trigger symptoms, including consciously shifting attention away from those reminders to more positive feelings, thoughts, goals, and choices. TFCBT is the adaptation of usual cognitive behavioral therapy to traumatic events. It places a focus on the traumatic event itself and on symptom relief by shifting how the patient thinks about the event, eg, how much the patient blames themselves and how that impacts their mood and other symptoms. Both are easy-to-learn approaches for clinicians who have an interest in doing this in the office.
CCPR: How do you deal with children who come into the emergency room with suicidality?
Dr. Ahmadi: It depends on how severe the symptoms are. In our emergency care unit, we sometimes need to transfer the child with PTSD and suicidality to an inpatient unit for further stabilization. On the other hand, even when children present with suicidal ideation, we can sometimes come up with a good suicide prevention plan that allows them to go home. We’ve actually published a study on suicide prevention (Ahmadi N et al, J Am Acad Child Adolesc Psychiatry 2020;59(10):S251–S252). The technique is derived from RFPP, and we call it RFPP-S (reminder-focused positive psychiatry and suicide prevention intervention).
CCPR: Can you tell us more about RFPP-S?
Dr. Ahmadi: RFPP-S is a brief, 2-day program that typically occurs while the child is in the emergency room. It consists of two 10-minute-long therapy sessions per day. These are behavioral modules focused on self-compassion, treatment engagement, increased ability to manage trauma reminders, distress tolerance, and safety planning skills. Adolescents with PTSD and suicidal ideation receive 10 minutes of RFPP-S modules twice a day for 2 consecutive days. There is also one 10-minute RFPP-S parent psychoeducation module. We used the Columbia-Suicide Severity Rating Scale (C-SSRS) as our outcome variable and found that the scores dropped from an average of 3.5–4.5 at baseline to 1.5–2.5 on the second day. This was followed by discharging from the emergency room and post-discharge outpatient management (Ahmadi N, J Am Acad Child Psy 2019;58(10):S269).
CCPR: What did the research show?
Dr. Ahmadi: Our study was a retrospective nested matched case-control study of 50 children with PTSD and suicidality who received RFPP-S and 150 children with PTSD and suicidality who did not receive RFPP-S during their 2-day psychiatric ER treatment visit. We found that the technique was significantly more effective than treatment as usual. There was a 55% reduction in PTSD symptoms vs only 10% in usual treatment, and there were clinically meaningful reductions in suicidality scores in 80% of those in the treatment group vs only 15% in usual treatment. The 1-month readmissions for suicidality for those getting RFPP-S was 0 compared to 205 (some patients had multiple readmissions).
CCPR: Thanks again for your time, gentlemen.
Editor’s note: Training in TFCBT is available at a nominal cost at www.NCTSN.org. Dr. Ahmadi plans to develop more training programs for RFPP-S in the near term.
Child PsychiatryDr. Steinberg: I’m the Associate Director of the National Center for Child Traumatic Stress at UCLA.
Dr. Ahmadi: I’m Assistant Professor of Psychiatry at UCLA and Director of Family Trauma Distress at Olive View, and Dr. Steinberg and I worked together with colleagues to develop our UCLA Brief COVID-19 Screen for Child/Adolescent PTSD.
CCPR: What is the National Center for Child Traumatic Stress? What’s its purpose?
Dr. Steinberg: The problem of child traumatic stress in the US is enormous: sexual abuse, physical abuse, neglect, domestic violence, and mixtures of complex trauma histories—including kids who are exposed to natural and manmade disasters, catastrophic school violence, community violence, exploitation, trafficking, traumatic bereavement, and so on. That’s the reason for the National Child Traumatic Stress Network Initiative: to make all systems that provide care and services to children and families more trauma informed, to ask about trauma histories and PTSD, and to help these kids receive needed assessments and evidence-based interventions.
CCPR: What are some of the symptoms of pandemic-associated trauma in children? And how do you assess for these symptoms?
Dr. Ahmadi: In our current pandemic, the trauma is often related to losses and traumatic events even when the child is unlikely to have COVID. Many youths have traumatic experiences related to COVID, like having someone close to you die from COVID—a family member, schoolmate, or teacher—or having a parent working in an environment where they’re exposed to the illness or where there’s been a quarantine in the family. Our new screening instrument can help clinicians assess these concerns more specifically for better treatment planning. (Editor’s note: The UCLA Brief COVID-19 Screen for Child/Adolescent PTSD is available at no cost in both English and Spanish for use by professionals across a range of child-serving systems, including behavioral health, primary care, pediatrics, schools, child welfare, juvenile justice, and residential care. See www.tinyurl.com/uv4qu5gr.)
CCPR: Is there research specifically on the effects of COVID on mental health?
Dr. Steinberg: We know from global reports of the pandemic that many adults and children have traumatic and stress symptoms due to COVID. When you assess kids who suffer from trauma, you usually expect maybe 10% or 20% to have PTSD. In April 2020, we saw an influx of adults and children coming with much more dysregulation, and we found 20%–40% of these people had PTSD related to the pandemic, which was kind of a shock to us. This is really important because the current standard of care for trauma screening is very limited in scope.
CCPR: How do you treat children with pandemic-related PTSD?
Dr. Ahmadi: In addition to usual trauma-informed care—such as helping kids get back to familiar routines, supporting structure and new routines when that’s not possible, and supporting parents and other caregivers so they can be present and supportive and reassuring to kids—we have used two techniques that show a lot of promise. One is called “reminder-focused positive psychiatry” (RFPP) and the other is called “trauma-focused cognitive behavioral therapy” (TFCBT). RFPP is focused on helping patients identify and manage reminders of trauma that trigger symptoms, including consciously shifting attention away from those reminders to more positive feelings, thoughts, goals, and choices. TFCBT is the adaptation of usual cognitive behavioral therapy to traumatic events. It places a focus on the traumatic event itself and on symptom relief by shifting how the patient thinks about the event, eg, how much the patient blames themselves and how that impacts their mood and other symptoms. Both are easy-to-learn approaches for clinicians who have an interest in doing this in the office.
CCPR: How do you deal with children who come into the emergency room with suicidality?
Dr. Ahmadi: It depends on how severe the symptoms are. In our emergency care unit, we sometimes need to transfer the child with PTSD and suicidality to an inpatient unit for further stabilization. On the other hand, even when children present with suicidal ideation, we can sometimes come up with a good suicide prevention plan that allows them to go home. We’ve actually published a study on suicide prevention (Ahmadi N et al, J Am Acad Child Adolesc Psychiatry 2020;59(10):S251–S252). The technique is derived from RFPP, and we call it RFPP-S (reminder-focused positive psychiatry and suicide prevention intervention).
CCPR: Can you tell us more about RFPP-S?
Dr. Ahmadi: RFPP-S is a brief, 2-day program that typically occurs while the child is in the emergency room. It consists of two 10-minute-long therapy sessions per day. These are behavioral modules focused on self-compassion, treatment engagement, increased ability to manage trauma reminders, distress tolerance, and safety planning skills. Adolescents with PTSD and suicidal ideation receive 10 minutes of RFPP-S modules twice a day for 2 consecutive days. There is also one 10-minute RFPP-S parent psychoeducation module. We used the Columbia-Suicide Severity Rating Scale (C-SSRS) as our outcome variable and found that the scores dropped from an average of 3.5–4.5 at baseline to 1.5–2.5 on the second day. This was followed by discharging from the emergency room and post-discharge outpatient management (Ahmadi N, J Am Acad Child Psy 2019;58(10):S269).
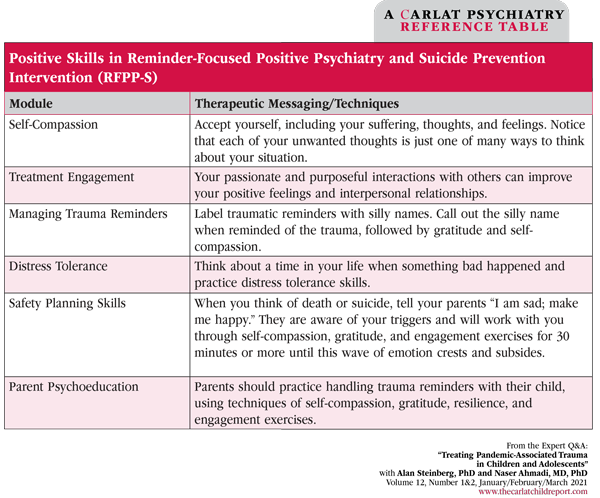
Table: Positive Skills in Reminder-Focused Positive Psychiatry and Suicide Prevention Intervention (RFPP-S)
(Click to view full-sized PDF.)
CCPR: What did the research show?
Dr. Ahmadi: Our study was a retrospective nested matched case-control study of 50 children with PTSD and suicidality who received RFPP-S and 150 children with PTSD and suicidality who did not receive RFPP-S during their 2-day psychiatric ER treatment visit. We found that the technique was significantly more effective than treatment as usual. There was a 55% reduction in PTSD symptoms vs only 10% in usual treatment, and there were clinically meaningful reductions in suicidality scores in 80% of those in the treatment group vs only 15% in usual treatment. The 1-month readmissions for suicidality for those getting RFPP-S was 0 compared to 205 (some patients had multiple readmissions).
CCPR: Thanks again for your time, gentlemen.
Editor’s note: Training in TFCBT is available at a nominal cost at www.NCTSN.org. Dr. Ahmadi plans to develop more training programs for RFPP-S in the near term.


Issue Date: March 12, 2021
Table Of Contents
Recommended
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2026 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



