Home » Nutritional Psychiatry in Practice
Nutritional Psychiatry in Practice
November 5, 2021
From The Carlat Psychiatry Report
 Drew Ramsey, MD.
Drew Ramsey, MD.
Assistant clinical professor of psychiatry at Columbia University, founder of the Brain Food Clinic, and the author of four books on nutrition and mental health, including 2021’s Eat to Beat Depression and Anxiety (HarperWave). Dr. Ramsey has disclosed no relevant financial or other interests in any commercial companies pertaining to this educational activity.
TCPR: Why should we talk about diet with our patients?
Dr. Ramsey: I am an avid practitioner of psychotherapy and psychopharmacology, but we often need more tools to help our patients, and there is a lot of science behind nutritional psychiatry. There are now three randomized trials showing that people with depression can benefit by shifting to a Mediterranean-style diet. In the SMILES trial, 32% of patients achieved full remission after changing their diet, compared to 8% of controls (Jacka FN et al, BMC Med 2017;15(1):23). Food is also a way to engage patients, and it puts us in the business of preventative mental health.
TCPR: Depression tends to improve when patients take on a new challenge. How did these studies control for that?
Dr. Ramsey: The trials used controls that have modest antidepressant effects on their own. In the SMILES trial, the control was a nondirective, supportive “befriending” therapy. That trial also looked at whether changes in weight, exercise, smoking, or self-efficacy predicted the improvements in depression, and they did not. The HELFIMED trial delivered the nutritional intervention in a group format, and the control was an activities group that played games and planned outings together (Parletta N et al, Nutr Neurosci 2019;22(7):474–487). There is also a negative study on whether nutritional counseling and/or a multinutrient supplement could prevent depression better than placebo in obese patients (Bot M, JAMA 2019;321(9):858–868).
TCPR: Are there other disorders besides depression where nutritional psychiatry is making headway?
Dr. Ramsey: There’s some evidence from the SMILES trial that the Mediterranean-style diet improves anxiety, and that’s something I’ve seen in my own practice. Also, we’ve seen some evidence in ADHD. A recent trial looked at the DASH diet (a diet for hypertension that is similar to the Mediterranean approach) in childhood ADHD. The children were not taking any stimulants, and their ADHD symptoms improved after four months with the diet. The placebo was a nonspecific dietary intervention that guided them to eat a certain amount of protein, fat, and carbohydrates (Khoshbakht Y et al, Eur J Nutr 2021;60(7):3647–3658).
TCPR: What goes into the Mediterranean diet?
Dr. Ramsey: The changes don’t have to be grand. In the SMILES trial, participants ate one more seafood meal a week, an extra half-serving of fruit a day, an extra serving of vegetables a day, and a couple more servings of beans a week. They ate more nuts, olive oil, and whole grains. The bigger change was in what they dropped, each week eating 21 fewer meals of highly processed foods, like fried, sugary, or “fast” foods and simple carbs.
TCPR: Do you have to be a nutritionist to do this work?
Dr. Ramsey: All mental health clinicians can make use of this. I’ve seen positive results in my own practice, where we run a training program in nutritional psychiatry, and you can see it in the research. One trial just used a 13-minute video on the Mediterranean diet followed by two five-minute phone calls, and even this minimal level of human contact was enough to reduce depression (Francis HM et al, PLoS One 2019;14(10):e0222768).
TCPR: What are some easy ways for patients to start this work?
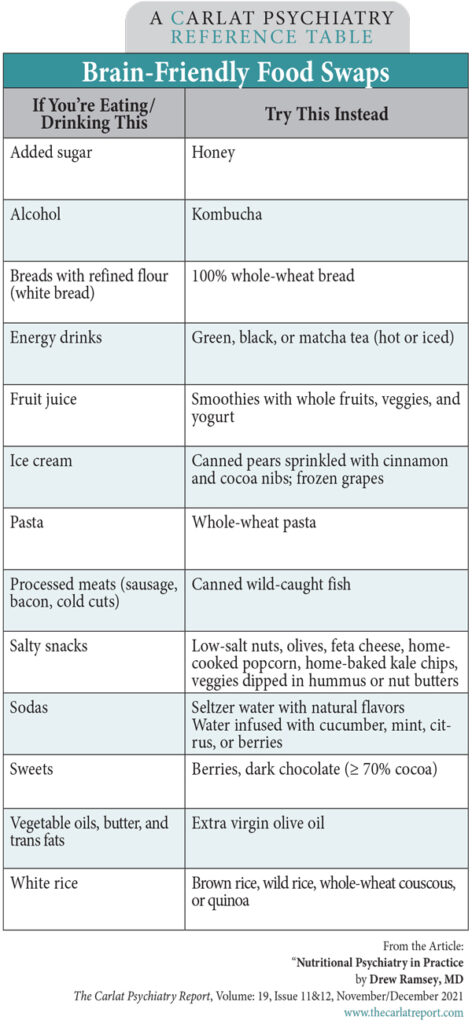
Dr. Ramsey: One of my most common prescriptions is raw, unsalted nuts. People worry that nuts are calorically dense, and they are filling, but they are also packed with nutrients—full of fiber, protein, minerals, healthy fats, and slow-burning carbohydrates. (Editor’s note: See the Brain-Friendly Food Swaps table on page 8 for more ideas.) Also look for foods they can get rid of, like simple sugars, sodas, and processed foods. And be careful about diet sodas and artificial sweeteners. Those just lead people to crave more sweet stuff, and they are associated with higher rates of depression and—in animals—hippocampal damage (Guo X et al, PLoS One 2014;9(4):e94715). I’d also get rid of all low-fat products, sugary breakfast cereals, and fried foods. If you have fried food, pan-fry at lower heat and use extra virgin olive oil (EVOO) or avocado oil.
TCPR: Why those oils?
Dr. Ramsey: EVOO is mostly a monounsaturated healthy fat, with phytonutrients that have antioxidant properties. Avocado oil is also good, but EVOO is less expensive and has more robust data. EVOO was included in the studies I’ve mentioned, and it also lowered depression on its own in a new trial that randomized people with depression to use 1.5–2 tablespoons per day of either EVOO or sunflower oil in their diet (Foshati S et al, J Acad Nutr Diet 2021; Epub ahead of print).
TCPR: What are “processed foods”?
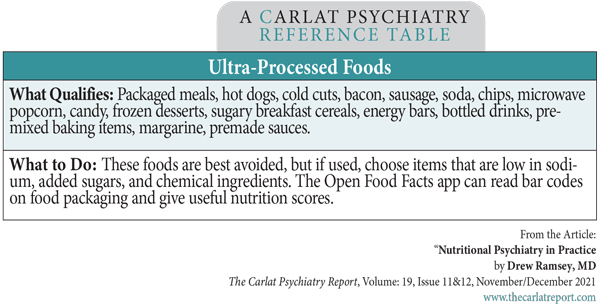
Dr. Ramsey: Technically, any food that has been cooked, dried, or modified from its original form is processed. But what we’re concerned with are ultra-processed foods. These tend to involve technologies that weren’t available 100 years ago. (Editor’s note: See the Ultra-Processed Foods table on page 8.) They are high in calories, low in nutrients, and have flavor and texture enhancers that make people want to eat more and more.
TCPR: What type of patient would benefit most from nutritional interventions?
Dr. Ramsey: The data are largely focused on depression, but nutritional psychiatry is useful to patients struggling with anxiety, addiction, and even psychosis. Patients who are interested in nutrition are often more motivated, but the biggest impact is likely for those who are totally disengaged from food. One misconception is that nutritional psychiatry is only for patients with mild disorders. In the HELFIMED trial, 86% had severe depression.
TCPR: How directive are you with patients?
Dr. Ramsey: I try to be neutral and respect patient autonomy and individuality. We are all unique in our tastes, preferences, and morals about food, so I find it best to recommend broad categories. Thus my mantra these days is: “Seafood, greens, nuts and beans, and a little dark chocolate.” That is a good start. We also focus on restoring a joyful relationship with food.
TCPR: Does depression get in the way of this work?
Dr. Ramsey: Yes, particularly problems with motivation, organization, and executive functioning—and also guilt. It can be overwhelming to think every meal is going to affect your mental health, and we don’t want this food work to be another burden. Too much focus on food can derail other aspects of treatment. Skills and finances can also get in the way. Not everybody knows how to cook seafood or can afford fresh fish. Still, this work can be done on a low budget. In the SMILES trial, this diet actually lowered participants’ food costs by more than $100 per month.
TCPR: Have there been further refinements beyond the Mediterranean approach?
Dr. Ramsey: Research is focusing on fermented foods, which improve the health and diversity of the gut microbiome. There are dozens of studies that associate poor microbiome health with mental illnesses, including depression, bipolar, schizophrenia, addiction, and autism. When the microbiome improves, those disorders tend to improve, perhaps by decreasing inflammation. Many people use a probiotic supplement, but I prefer food sources. A serving of kefir has several hundred times the colony-forming units of a probiotic capsule.
TCPR: Are some foods particularly challenging for patients?
Dr. Ramsey: Seafood can be a struggle. Some patients just don’t like it, but I’ve found shrimp, smoked salmon, and even canned seafood to be good entry points. Others have concerns about mercury, microplastics, and other pollutants. Small fish like anchovies and sardines are relatively free of environmental toxins and are a great source of omega-3. Meat and seafood also raises ethical concerns for some, and we need to respect those stances.
TCPR: How do you modify the diet for vegetarians and vegans?
Dr. Ramsey: To start with, we need to understand where plant-based folks are coming from, as they’ve often faced opposition in the healthcare system. The concerns I have for patients on plant-based diets are low intakes of B-12, zinc, iron, and long-chain omega-3 fatty acids. We can test for some of those and, of course, supplement if needed. Many cereals and other foods are supplemented with these and marketed to vegetarians and vegans. Omega-3s are more challenging. Flax seeds have short-chain omega-3s like ALA, but the brain needs long-chain ones like EPA and DHA. Some patients following plant-based diets eat bivalves like clams and mussels, which contain omega-3s. Others take supplements, but keep in mind the omega-3 supplements that work in depression have a higher ratio (≥ 60%) of EPA, and those are all derived from fish (Sublette ME, J Clin Psychiatry 2011;72(12):1577–1584).
TCPR: Can you do this work with patients who have eating disorders?
Dr. Ramsey: We don’t have research on that, but I wouldn’t encourage it. Eating disorder therapies tend to help patients not think about food choices too much, and nutritional psychiatry revolves around getting people to deeply engage and think around their food. We don’t want nutritional psychiatry to be used as a proxy for disordered eating.
TCPR: How can clinicians get training in nutritional psychiatry?
Dr. Ramsey: The American Psychiatric Association hosts trainings at their annual meetings, and our team has a digital training program at drewramseymd.com.
TCPR: Thank you for your time, Dr. Ramsey.
General PsychiatryDr. Ramsey: I am an avid practitioner of psychotherapy and psychopharmacology, but we often need more tools to help our patients, and there is a lot of science behind nutritional psychiatry. There are now three randomized trials showing that people with depression can benefit by shifting to a Mediterranean-style diet. In the SMILES trial, 32% of patients achieved full remission after changing their diet, compared to 8% of controls (Jacka FN et al, BMC Med 2017;15(1):23). Food is also a way to engage patients, and it puts us in the business of preventative mental health.
TCPR: Depression tends to improve when patients take on a new challenge. How did these studies control for that?
Dr. Ramsey: The trials used controls that have modest antidepressant effects on their own. In the SMILES trial, the control was a nondirective, supportive “befriending” therapy. That trial also looked at whether changes in weight, exercise, smoking, or self-efficacy predicted the improvements in depression, and they did not. The HELFIMED trial delivered the nutritional intervention in a group format, and the control was an activities group that played games and planned outings together (Parletta N et al, Nutr Neurosci 2019;22(7):474–487). There is also a negative study on whether nutritional counseling and/or a multinutrient supplement could prevent depression better than placebo in obese patients (Bot M, JAMA 2019;321(9):858–868).
TCPR: Are there other disorders besides depression where nutritional psychiatry is making headway?
Dr. Ramsey: There’s some evidence from the SMILES trial that the Mediterranean-style diet improves anxiety, and that’s something I’ve seen in my own practice. Also, we’ve seen some evidence in ADHD. A recent trial looked at the DASH diet (a diet for hypertension that is similar to the Mediterranean approach) in childhood ADHD. The children were not taking any stimulants, and their ADHD symptoms improved after four months with the diet. The placebo was a nonspecific dietary intervention that guided them to eat a certain amount of protein, fat, and carbohydrates (Khoshbakht Y et al, Eur J Nutr 2021;60(7):3647–3658).
TCPR: What goes into the Mediterranean diet?
Dr. Ramsey: The changes don’t have to be grand. In the SMILES trial, participants ate one more seafood meal a week, an extra half-serving of fruit a day, an extra serving of vegetables a day, and a couple more servings of beans a week. They ate more nuts, olive oil, and whole grains. The bigger change was in what they dropped, each week eating 21 fewer meals of highly processed foods, like fried, sugary, or “fast” foods and simple carbs.
TCPR: Do you have to be a nutritionist to do this work?
Dr. Ramsey: All mental health clinicians can make use of this. I’ve seen positive results in my own practice, where we run a training program in nutritional psychiatry, and you can see it in the research. One trial just used a 13-minute video on the Mediterranean diet followed by two five-minute phone calls, and even this minimal level of human contact was enough to reduce depression (Francis HM et al, PLoS One 2019;14(10):e0222768).
TCPR: What are some easy ways for patients to start this work?
Dr. Ramsey: One of my most common prescriptions is raw, unsalted nuts. People worry that nuts are calorically dense, and they are filling, but they are also packed with nutrients—full of fiber, protein, minerals, healthy fats, and slow-burning carbohydrates. (Editor’s note: See the Brain-Friendly Food Swaps table on page 8 for more ideas.) Also look for foods they can get rid of, like simple sugars, sodas, and processed foods. And be careful about diet sodas and artificial sweeteners. Those just lead people to crave more sweet stuff, and they are associated with higher rates of depression and—in animals—hippocampal damage (Guo X et al, PLoS One 2014;9(4):e94715). I’d also get rid of all low-fat products, sugary breakfast cereals, and fried foods. If you have fried food, pan-fry at lower heat and use extra virgin olive oil (EVOO) or avocado oil.
TCPR: Why those oils?
Dr. Ramsey: EVOO is mostly a monounsaturated healthy fat, with phytonutrients that have antioxidant properties. Avocado oil is also good, but EVOO is less expensive and has more robust data. EVOO was included in the studies I’ve mentioned, and it also lowered depression on its own in a new trial that randomized people with depression to use 1.5–2 tablespoons per day of either EVOO or sunflower oil in their diet (Foshati S et al, J Acad Nutr Diet 2021; Epub ahead of print).
TCPR: What are “processed foods”?
Dr. Ramsey: Technically, any food that has been cooked, dried, or modified from its original form is processed. But what we’re concerned with are ultra-processed foods. These tend to involve technologies that weren’t available 100 years ago. (Editor’s note: See the Ultra-Processed Foods table on page 8.) They are high in calories, low in nutrients, and have flavor and texture enhancers that make people want to eat more and more.
Table: Ultra-Processed Foods
(Click to view full-sized PDF.)
TCPR: What type of patient would benefit most from nutritional interventions?
Dr. Ramsey: The data are largely focused on depression, but nutritional psychiatry is useful to patients struggling with anxiety, addiction, and even psychosis. Patients who are interested in nutrition are often more motivated, but the biggest impact is likely for those who are totally disengaged from food. One misconception is that nutritional psychiatry is only for patients with mild disorders. In the HELFIMED trial, 86% had severe depression.
TCPR: How directive are you with patients?
Dr. Ramsey: I try to be neutral and respect patient autonomy and individuality. We are all unique in our tastes, preferences, and morals about food, so I find it best to recommend broad categories. Thus my mantra these days is: “Seafood, greens, nuts and beans, and a little dark chocolate.” That is a good start. We also focus on restoring a joyful relationship with food.
TCPR: Does depression get in the way of this work?
Dr. Ramsey: Yes, particularly problems with motivation, organization, and executive functioning—and also guilt. It can be overwhelming to think every meal is going to affect your mental health, and we don’t want this food work to be another burden. Too much focus on food can derail other aspects of treatment. Skills and finances can also get in the way. Not everybody knows how to cook seafood or can afford fresh fish. Still, this work can be done on a low budget. In the SMILES trial, this diet actually lowered participants’ food costs by more than $100 per month.
TCPR: Have there been further refinements beyond the Mediterranean approach?
Dr. Ramsey: Research is focusing on fermented foods, which improve the health and diversity of the gut microbiome. There are dozens of studies that associate poor microbiome health with mental illnesses, including depression, bipolar, schizophrenia, addiction, and autism. When the microbiome improves, those disorders tend to improve, perhaps by decreasing inflammation. Many people use a probiotic supplement, but I prefer food sources. A serving of kefir has several hundred times the colony-forming units of a probiotic capsule.
TCPR: Are some foods particularly challenging for patients?
Dr. Ramsey: Seafood can be a struggle. Some patients just don’t like it, but I’ve found shrimp, smoked salmon, and even canned seafood to be good entry points. Others have concerns about mercury, microplastics, and other pollutants. Small fish like anchovies and sardines are relatively free of environmental toxins and are a great source of omega-3. Meat and seafood also raises ethical concerns for some, and we need to respect those stances.
TCPR: How do you modify the diet for vegetarians and vegans?
Dr. Ramsey: To start with, we need to understand where plant-based folks are coming from, as they’ve often faced opposition in the healthcare system. The concerns I have for patients on plant-based diets are low intakes of B-12, zinc, iron, and long-chain omega-3 fatty acids. We can test for some of those and, of course, supplement if needed. Many cereals and other foods are supplemented with these and marketed to vegetarians and vegans. Omega-3s are more challenging. Flax seeds have short-chain omega-3s like ALA, but the brain needs long-chain ones like EPA and DHA. Some patients following plant-based diets eat bivalves like clams and mussels, which contain omega-3s. Others take supplements, but keep in mind the omega-3 supplements that work in depression have a higher ratio (≥ 60%) of EPA, and those are all derived from fish (Sublette ME, J Clin Psychiatry 2011;72(12):1577–1584).
TCPR: Can you do this work with patients who have eating disorders?
Dr. Ramsey: We don’t have research on that, but I wouldn’t encourage it. Eating disorder therapies tend to help patients not think about food choices too much, and nutritional psychiatry revolves around getting people to deeply engage and think around their food. We don’t want nutritional psychiatry to be used as a proxy for disordered eating.
TCPR: How can clinicians get training in nutritional psychiatry?
Dr. Ramsey: The American Psychiatric Association hosts trainings at their annual meetings, and our team has a digital training program at drewramseymd.com.
TCPR: Thank you for your time, Dr. Ramsey.
Table: Brain-Friendly Food Swaps
(Click to view full-sized PDF.)
KEYWORDS alternative-treatments complimentary-medicine dash-diet natural-treatments nutrition therapy-during-medication-appointment

Issue Date: November 5, 2021
Table Of Contents
Recommended
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2026 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



