Dissociative Identity Disorder vs Plural Identity in Teens and Young Adults

CCPR: What is dissociative identity disorder (DID)?
Dr. Mitra: The DSM-5 diagnostic criteria for DID includes two or more distinct personalities, each with the sense of consciousness and memory. Each personality can have its own mood and stress responses. Since there is more than one personality, there are gaps in memory and recollection of day-to-day events. This is due to shifts in consciousness from one personality to another. Patients with DID also have trouble functioning in the community, in relationships, at work, etc.
CCPR: How common is DID?
Dr. Mitra: DID occurs in 1%–1.5% of adults, but we don’t have numbers for children and adolescents (Sar V, Epidemiol Res Int 2011;2011:404538). Patients can be in the mental health system for five to 12 years before they formally get a diagnosis of DID (Spiegel D et al, Depression and Anxiety 2011;28(9):824–852). Kids might not be diagnosed until they are adults.
CCPR: What makes it difficult to spot?
Dr. Mitra: DID can overlap with personality disorders, mood disorders, or psychotic disorders. Gaps in recall happen in borderline personality disorder, with dissociation and inability to recall events especially in the context of mood dysregulation. People with PTSD may also experience cognitive dissonance and be unable to recall certain events.
CCPR: How are memory gaps different in DID versus other conditions?
 Dr. Mitra: In DID, patients experience two or more personality states with a distinct discontinuity between each. Memory loss in PTSD is often fragmented and related to the trauma. Memory loss in DID can involve traumatic memories but also loss of day-to-day events, personal information, or even the date and time. With borderline personality disorder, some form of continuity is evident.
Dr. Mitra: In DID, patients experience two or more personality states with a distinct discontinuity between each. Memory loss in PTSD is often fragmented and related to the trauma. Memory loss in DID can involve traumatic memories but also loss of day-to-day events, personal information, or even the date and time. With borderline personality disorder, some form of continuity is evident.
CCPR: Can patients control the shifts between personalities in DID?
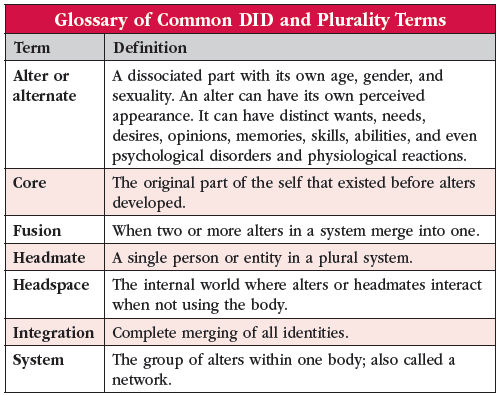
Dr. Mitra: No. You sometimes see a trance-like moment, or rolling of eyes, with a switch of alters that happens quite suddenly (Editor’s note: For more information on alters, see table below).
CCPR: What do we know about the etiology of DID?
Dr. Mitra: DID is associated with childhood trauma and abuse, a strong tendency toward fantasy-based thinking, the ability to dissociate, media influences, social isolation, and therapist expectations or orientation (Mitra P and Jain A. Dissociative Identity Disorder. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2022). Kluft describes four predisposing factors for DID (Kluft RP, Psychoanalyt Inquiry 2000;20(2):259–286). Factor one is how well the person learned to dissociate in the face of factor two: traumatic childhood experiences. Factor three is lack of stable external emotional support and validation. All three of these factors theoretically combine to create the fourth factor, which is the presence of independent alters with distinct names and identities.
CCPR: How is the teen and young adult social media phenomenon of plural identity different from DID?
Dr. Mitra: Plural identity is not recognized in the DSM-5. The concept came into social media after the DSM-5 published the current version of DID. As of 2021, one TikTok community called “A System” had 1.1 million followers, and there were 910 million views on the hashtag #did. In plural identity or multiplicity, the alters refer to themselves as “headmates” or “system mates.” They are co-conscious of each other, and they generally remember the events that happen during a day. Presumably there’s less strongly partitioned memory, and the person can function in day-to-day life, work, and relationships. This contrasts with DID, where there are memory gaps. People who identify as plurals state that they can switch consciously between headmates. In DID, the switching happens in response to a traumatic event or a stressor that can cause one alter to come in and the other to go out.
CCPR: Is there research on plural identity?
Dr. Mitra: While there is no real research on plural identity per se, there is growing research literature on internal family systems therapy (IFST), which has been around since the 1990s. IFST posits that all of us contain within us entire tribes of fully formed personalities (“parts”) that ideally work together much like a plural system. When they are not getting along, there are symptoms such as depression and anxiety. Therapy involves identifying and sorting out the relationships between parts.
CCPR: How do DID and plural identity differ in their functional impact on the person?
Dr. Mitra: DID implies impaired function, and treatment aims to make the alters conscious of each other and form one integrated whole. Persons with plural identity see it as their way of being. They are functional in their day-to-day life. They may come to treatment for another condition, such as depression, but not to integrate their headmates. They see plurality as a form of diversity, not a disorder. To distinguish between the two, we might ask if the different entities share memories. Is the person suffering from the impact of having different personalities, or are they content with having headmates? Focus on function, including academically and socially. Also explore their use of social media. This may impact their cognition and sense of identity (Ribáry G et al, Front Psychol 2017;8:938).
CCPR: Are there scales to help us differentiate DID from other conditions?
Dr. Mitra: The Dissociative Experiences Scale is a 28-item self-reported instrument whose items tap primarily absorption, imaginative involvement, depersonalization, derealization, and amnesia (Bernstein EM and Putnam FW, J Nerv Ment Dis 1986;174(12):727–735). The Dissociation Questionnaire is 63 questions and measures identity confusion and fragmentation, loss of control, amnesia, and absorption (Vanderlinden J et al, Clin Psychol Psychother 1993;1(1):21–27). The Difficulties in Emotion Regulation Scale is a 36-item self-reported measure of nonacceptance of emotional responses, difficulties engaging in goal-directed behavior, impulse control difficulties, and lack of emotional awareness (Hallion LS et al, Front Psychol 2018;9:539). Other tools include the Minnesota Multiphasic Personality Inventory as well as the Posttraumatic Diagnostic Scale for DSM-5 (Editor’s note: For more information, see table). These scales, dissociative disorders, and combinations of the two. 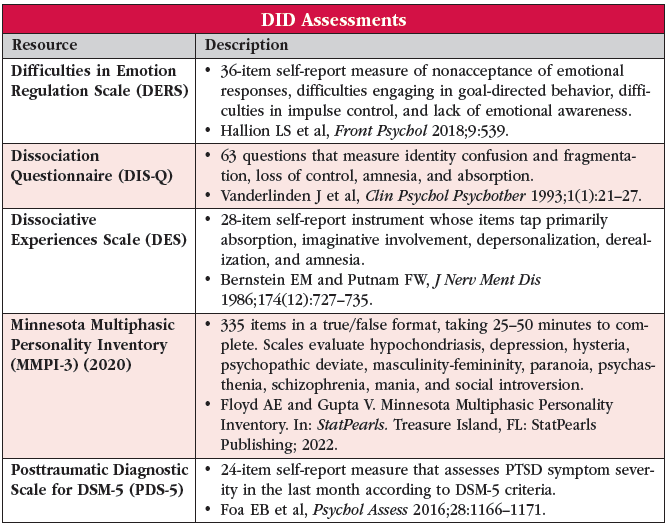
CCPR: How do families respond to DID and plural identity?
Dr. Mitra: Both DID and plurality are difficult to explain to families. The amnesia between personalities in DID is particularly confusing. In my experience, families also struggle with the person’s lack of insight into their own shifting between identities. With plural identity, there are similarities to gender diversity. For example, folks with plurality or multiplicity use terms like “coming out,” revealing themselves to the outside world as a multiple, with pronoun choices such as they/them. The vocabulary around plurality can be challenging for families to process and accept.
CCPR: Tell us more about treatment of DID.
Dr. Mitra: Treatment for DID is a three-pronged approach: 1) Make sure that folks are safe and stable, addressing such things as mood disorders and self-injurious behaviors; 2) Confront, work through, and integrate traumatic memories (this is challenging because it means working with different alters that have different memories and moments of amnesia); and 3) Integrate all the identities of the alters or personalities into one and rehabilitate the one person in day-to-day activities.
CCPR: Do patients with DID usually want to integrate their personalities?
Dr. Mitra: No. Be mindful of the patient’s goals, which might not be an integrated personality. Patients may want to address mood and anxiety and not the memory gaps, the shifting between alters, or the dysfunction that they experience from those. Meet the patient where they are—the goal of the moment is OK.
CCPR: Are there specific treatment modalities that help in the treatment of DID?
Dr. Mitra: Many DID patients are considered auto-hypnotic, and hypnosis has some efficacy (Kluft RP, Psychiatr Med 1992;10(4):31–46). Eye movement desensitization and reprocessing (EMDR) can be used with different identities to reduce symptoms, especially mood symptoms, and to strengthen the ego (Paulson S. Treating Dissociative Identity Disorder with EMDR, Ego State Therapy, and Adjunct Approaches, In: Forgash C and Copeley M, ed. Healing the Heart of Trauma and Dissociation With EMDR and Ego State Therapy. New York, NY: Springer Publishing; 2007:141–180). Lee et al published an excellent case study that includes the patient’s art and cultural perspectives (Lee SH et al, Soa Chongsonyon Chongsin Uihak 2022;33(3):73–81).
CCPR: Can medications help in the treatment of DID?
Dr. Mitra: There are case studies but no larger-scale studies of medication treatment of DID. Many folks diagnosed with DID are prescribed medications like mood stabilizers, antipsychotics, or antidepressants. Certainly, an antidepressant like an SSRI for mood or PTSD might be helpful, but at this point, we do not have the data to support using medication primarily for DID. In any case, it is best to avoid benzodiazepines in this population (Gentile JP et al, Innov Clin Neurosci 2013;10(2):22–29).
CCPR: With gaps in time and amnesia for some memories, how do you help people stay safe?
Dr. Mitra: Have a support system in place that is aware of switches. Educate the family, teachers, and other caregivers about how stress can trigger a shift in alters. Track specific individualized stressors with the person. You might try to create an “in-network” system, where you talk with one personality, say an adult alter, to monitor another one, say of a child. Be aware of triggers and trauma and set up larger support systems. Community health workers can go to the home frequently to check on young adults who are living alone.
CCPR: Any final tips for helping patients with DID?
Dr. Mitra: Take time to come to a diagnosis, then learn about alters and the stressors that impact switching and ensure that folks are safe in the community. Promote stability of their relationships, support acceptance on the part of family and others, and ensure that you are mindful and respectful in your interactions.
CCPR: Thank you for your time, Dr. Mitra.
 Paroma Mitra, MD.
Paroma Mitra, MD. 

_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.jpg?1729528747)



