Controlled Substances: Handling Red Flags
Your college-age patient leaves you a voicemail: “I know you just refilled my Adderall, and I’m really sorry about this, but I accidentally spilled it down the sink.” They leave their pharmacy information and let you know that they have a “huge exam” in two days and “would appreciate an immediate refill.”
Is this an innocent request, or has a Trojan horse of misuse or diversion entered the doctor-patient relationship? Are you annoyed? Anxious? And how does your reaction change if this patient has other “red flags” for substance misuse?
In this article, I’ll review data regarding prescription misuse (ie, use outside of prescribed directions) and diversion (ie, medications getting into the hands of those they’re not prescribed to). I’ll focus on stimulants and benzodiazepines and cover best practices for prescribing scheduled medications, including policies to guide your response to scenarios like the one above.
Stimulants
ADHD is a risk factor for substance use disorders (SUDs), but stimulant therapy can reduce the likelihood of substance use in ADHD (Quinn PD et al, Am J Psychiatry 2017;174(9):877–885). That said, patients who misuse stimulants are more likely to use alcohol and other substances, and as many as 13% of patients who misuse stimulants have met criteria for an SUD. White and Hispanic college-age males with comorbid SUDs are the most likely to misuse or divert stimulants (Clemow DB and Walker DJ, Postgrad Med 2014;126(5):64–81). In one self-report, 8% of 9,100 college students reported a history of misusing stimulants—more than those who reported a legitimate prescribed use. Over half of college students who are prescribed stimulants report being solicited for diversion. Amphetamines are misused and diverted about four times more often than methylphenidates, and animal models confirm that amphetamines have more potent and rewarding dopaminergic effects (Clemow and Walker, 2014).
Most people who misuse stimulants do so to improve their concentration at school or work, but this may be a false hope. Studies in normal subjects yield mixed results, with some showing worse sleep and impaired next-day concentration after taking a stimulant (Tselha T et al, Behav Brain Res 2019;370:111940).
Up to 20% of the general adult population presenting for an ADHD evaluation may exaggerate symptoms with the goal of obtaining a stimulant prescription, and some studies have reported that this number is as high as 50% for college students. Getting an academic edge through medications, netting better campus accommodations as a result of an ADHD diagnosis, and desiring to misuse or sell medications are common motivations for malingering (Clemow and Walker, 2014).
Benzodiazepines
As with stimulants, white college-age adults with SUDs are the population most likely to misuse benzodiazepines (Votaw VR et al, Drug Alcohol Depend 2019;200:95–114). Misuse is often motivated by symptoms rather than recreation. Seventy-five percent of national survey respondents who admitted to misusing prescription tranquilizers reported doing so to treat anxiety or sleep (www.tinyurl.com/yyn2s662). Most of this misuse (69%) involved alprazolam, likely due to its rapid onset of action and unique propensity to increase striatal dopamine (Ait-Daoud N et al, J Addict Med 2018;12(1):4–10). After alprazolam, other drugs that rank high for misuse are clonazepam, diazepam, and lorazepam (Votaw et al, 2019).
Diverted benzodiazepines may only be one degree removed from your office: 20% of adolescents and adults with a benzodiazepine prescription reported diverting it to others. 80% of those who have reported misusing benzodiazepines said that they obtained diverted meds from a friend or family member with a prescription (Votaw et al, 2019).
Red flags
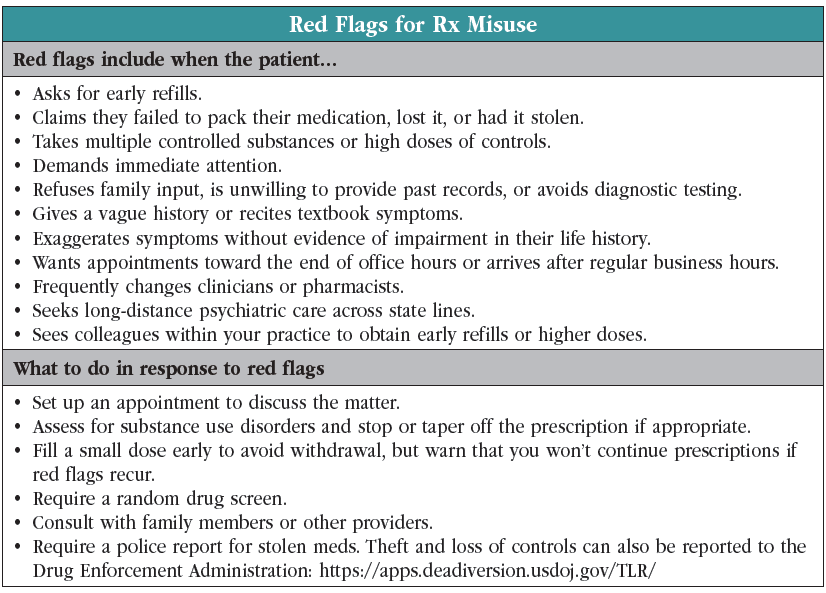
Warning signs for misuse or diversion include claims of lost or stolen medications, demands for immediate attention, and requests for specific medications. People may claim exaggerated, vague, or “textbook” symptoms, decline workups, and refuse permission to obtain prior medical records or collateral, which might include stating that they’re unavailable (https://apps.deadiversion.usdoj.gov/guidance; also see our “Red Flags for Rx Misuse” table on page 3).
As you evaluate red flags, keep in mind that implicit biases often cause us to treat some individuals differently. Implicit association testing of 300 psychiatrists, residents, fellows, and medical students, for example, revealed a significant link between Black faces and the concept of noncompliance (Tobon AL et al, Acad Psychiatry 2021;45(1):23–33). A universally applied, clearly communicated policy for starting and refilling controlled substances helps minimize the consequences of our implicit biases. Your policy should be discussed with patients and signed with the written treatment agreements that precede your first visit or first prescription.
Your controlled substance policy should include the standard conversation you have when starting any medication (for example, patient expectations for medications, likely outcomes, potential risks, and alternatives). The Carlat Report has a template policy at www.tinyurl.com/2n6zv6cs. As you adapt this template to your practice or craft your own, be sure to stipulate which red flags will cause you to stop or limit refills, how often you will provide an early refill and under what conditions, when you will require scheduled or random urine drug screens, and how often you will require follow-up appointments. Most states require pharmacists to log controlled prescriptions in a central database, and your policy should describe how you will use the state prescription monitoring program.
There is no algorithm for handling red flags. Talk with the patient (and collaterals, if needed) about your concerns, and refer the patient to your agreed-on policy as a guide for the next steps. Check your state’s prescription drug monitoring database, switch to e-prescribing, and consider whether a urine drug screen would be helpful. If you’re going to provide an early refill, you may limit it to just enough pills to get the patient to your next appointment.
 If you have confirmed that misuse or diversion is present, assess for an SUD and offer treatment if one is present. Stimulants can be stopped immediately, as the main withdrawal symptom is a non-dangerous fatigue. For benzodiazepines, initiate a taper to prevent seizures, and refer for inpatient detox if the patient has risk factors such as epilepsy, significant medical illness, a history of withdrawal complications, or comorbid SUDs such as alcohol or opioid use disorders.
If you have confirmed that misuse or diversion is present, assess for an SUD and offer treatment if one is present. Stimulants can be stopped immediately, as the main withdrawal symptom is a non-dangerous fatigue. For benzodiazepines, initiate a taper to prevent seizures, and refer for inpatient detox if the patient has risk factors such as epilepsy, significant medical illness, a history of withdrawal complications, or comorbid SUDs such as alcohol or opioid use disorders.
CARLAT VERDICT
Controlled medications require extra assessment and stricter prescribing practices. When prescribing controls, watch for red flags and have a policy that you apply fairly and equally to all. Offer treat- ment for SUDs when they arise.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



