Home » Becoming a Board-Certified Addiction Clinician
Becoming a Board-Certified Addiction Clinician
January 1, 2019
From The Carlat Addiction Treatment Report
 Michael Weaver, MD, FASAM
Michael Weaver, MD, FASAM
Professor and medical director at the Center for Neurobehavioral Research on Addictions at the University of Texas Medical School. Author of Addiction Treatment (Carlat Publishing, 2017). Dr. Weaver has disclosed that he has no relevant financial or other interests in any commercial companies pertaining to this educational activity.
CATR: To start off, could you tell us why a psychiatrist or any other physician would want to be board-certified in addiction?
Dr. Weaver: Patients with addiction are common in psychiatric or any other practice. You’re going to see patients who have these issues, so it’s good to be prepared and able to focus on treating addiction, as well as to be part of a growing group of specialists.
CATR: Are there opportunities that may open up for practitioners as a result of certification?
Dr. Weaver: The opioid crisis has opened the doors to an array of federal funding. And with funding for additional treatment outlets, there are going to be more positions for folks who are knowledgeable about addiction, and certification will eventually become a requirement for that. You can have practice opportunities in a variety of venues, from the more traditional residential focus to the currently popular medication treatment focus. You can also work with other formats such as multilevel specialty programs, freestanding addiction clinics, or even addiction clinics embedded within other practices. Practitioners can also gain recognition as experts in a growing subspecialty and assume leadership positions as administrators, educators, and policy consultants. All of this can open up earning potential.
CATR: There continues to be a tremendous need, and having that certification increases the chances of finding employment in any setting.
Dr. Weaver: Absolutely, and now that addiction medicine is recognized as a subspecialty by the American Board of Medical Specialties (ABMS), it is gaining more credence among medical practitioners. And, of course, addiction psychiatry has been an ABMS subspecialty for quite a while.
CATR: This leads us to an issue that is confusing for many practitioners. Could you tell us about the difference between board certification in addiction psychiatry and addiction medicine?
Dr. Weaver: These are two separate boards. To get certified in addiction psychiatry, you have to be board-certified in psychiatry and complete a 1-year addiction psychiatry fellowship. Addiction medicine is newer and more inclusive—you can come from any specialty, not just psychiatry, and there is no requirement for a fellowship, at least until 2021. Instead, there is a practice pathway, so psychiatrists who have been treating addiction but didn’t do a fellowship may have the opportunity to get board certification by virtue of their clinical practice.
CATR: Are there any differences in focus between addiction psychiatry and addiction medicine?
Dr. Weaver: The differences are pretty minor. Philosophically, addiction medicine may be a little bit broader in terms of addressing more potential medical complications, and may include more aspects of pain management or considerations related to obstetrics. So it may be a little bit more broad-based, but then anyone who has been doing addiction psychiatry for a while probably has encountered some of that in the course of their practice. Addiction psychiatry, on the other hand, has more of a focus on co-occurring psychiatric disorders.
CATR: Makes sense. Let’s talk about the process of board certification in addiction medicine—can you break it down?
Dr. Weaver: Sure. There are a couple of ways to do it, but across all those different pathways to certification in addiction medicine, you need to have certification in a primary board under ABMS. That can be psychiatry, internal medicine, pediatrics, obstetrics—any of those ABMS member boards.
CATR: And then you can do a fellowship or the practice pathway that you mentioned?
Dr. Weaver: Correct. So the fellowship pathway is pretty straightforward. You would do an addiction medicine fellowship. Those are in the process of being accredited by the Accreditation Council for Graduate Medical Education (ACGME), and there are 14 programs currently accredited. You can also complete one that has been accredited by the Addiction Medicine Foundation, formerly known as the American Board of Addiction Medicine and soon to be known as the American College of Academic Addiction Medicine. There are around 50 of those programs, and they also will count, because they basically followed the same guidelines that the ACGME is using.
CATR: Are these 1-year fellowships?
Dr. Weaver: Most of them are. Some institutions have either a requirement or an option for a research-focused 2-year fellowship, so you can do either, but you must do the full fellowship and complete it successfully in order to apply for certification. So if you do a 2-year fellowship, you’ve got to do both years before you apply. If you don’t complete the fellowship, you can count that toward the time in practice, but that would fall under the practice pathway.
CATR: Can you walk us through what the practice pathway is about?
Dr. Weaver: Sure. For the practice pathway, you need to have 1,920 hours of subspecialty-level addiction medicine–specific practice. And those 1,920 hours are basically the equivalent of 1 year’s full-time practice. However, that doesn’t have to be done over 1 year; it can be spread out over the 5 years prior to the time in which you apply for certification. Plus, it requires a minimum of 24 months in practice, so if you did 1 year full-time you wouldn’t meet the requirements; however, if you did 2 years half-time or full-time, then that would meet them. Also, these cannot be hours earned in residency training.
CATR: Do you need to primarily or exclusively treat addiction during these required hours?
Dr. Weaver: Well, you have to be able to describe the kind of addiction-specific practice that you are doing. You can count up to 25% of those 1,920 hours as addiction-specific practice within another primary specialty. For example, if you are doing family medicine and you’re addressing smoking cessation, or you are seeing people and doing motivational interviewing for alcohol use disorder, you can count up to 480 hours if you describe what you are doing consistently in a general practice.
CATR: What about the remaining 75% of the hours?
Dr. Weaver: The other 1,440 hours need to be in addiction medicine–specific practice, but this can include research or teaching. It’s just that 480 of those hours have to be hands-on patient care, so you can’t be doing all academics or all lab. At least 25% has to be hands-on patient care in addiction medicine.
CATR: Could you give us some examples of an addiction-specific practice?
Dr. Weaver: It can take a variety of forms. The simplest example a lot of people think of is prescribing buprenorphine and describing the number of patients and amount of time you spend doing that with patients, and what you do in addition to prescribing in terms of counseling, prevention, and addressing other comorbidities. It could also be spent part-time in a formal treatment facility, such as working as a staff physician or medical director for a residential program doing evaluations for current patients.
CATR: So this would need to be documented in the application. Is there any verification process?
Dr. Weaver: Yes. All of that would need to be verified by someone who is familiar with the individual’s practice—ideally, the direct supervisor, department chair, or chief of staff. But it could also be, for example, another physician in the community who has direct experience through cross-referral of patients, or collegial interactions through medical societies and professional meetings, or someone who works with the applicant who is not under the applicant’s direct supervision.
CATR: So if I were a clinician in private practice who screens every patient for addiction, treats comorbidities, and then treats some addiction directly, would that meet the requirement?
Dr. Weaver: That would count for up to 25% of the 1,920 hours. For the other 1,440 hours, you need to devote time specifically to doing addiction medicine activities separate from that, which could be all those things that I gave examples of earlier. Or you could work in a hospital detox unit or a dual-diagnosis unit, for example.
CATR: So those additional hours would have to be in an addiction specialty setting?
Dr. Weaver: In general, yes. If you’re saying, “Well, I just screen everybody and counsel everybody in my own general practice,” that’s really hard to justify.
CATR: What if I were doing, say, full-time buprenorphine practice in private practice? Would that qualify?
Dr. Weaver: You could say, “Well, here’s the time I set aside for doing that and here’s how many patients I see, and here’s what I do for them.” There’s not a set template for how people are doing these things—obviously there’s some latitude—so it depends on how well people describe what it is that they are doing.
CATR: OK. Let’s say I meet the criteria for the practice pathway and apply for certification. What happens next?
Dr. Weaver: That allows you to sit for the certification exam. The exam is offered at Prometric test centers with the National Board of Medical Examiners. There are about 300 centers in the US, so it’s similar to many other medical certification exams in that respect. It’s a computer-administered secure exam for the initial certification.
CATR: Can you give us some tips on how to prepare for the exam?
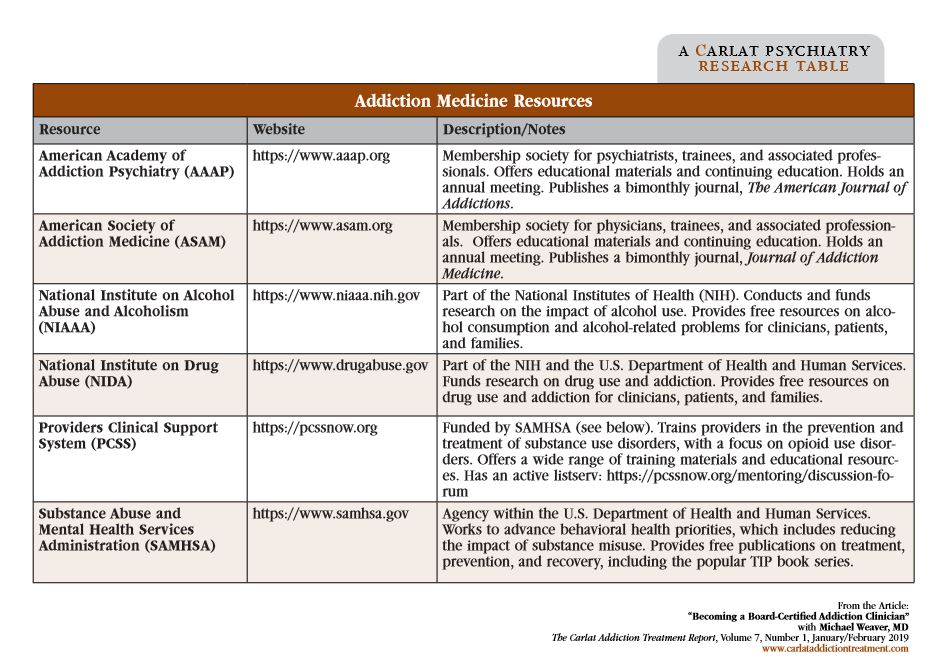
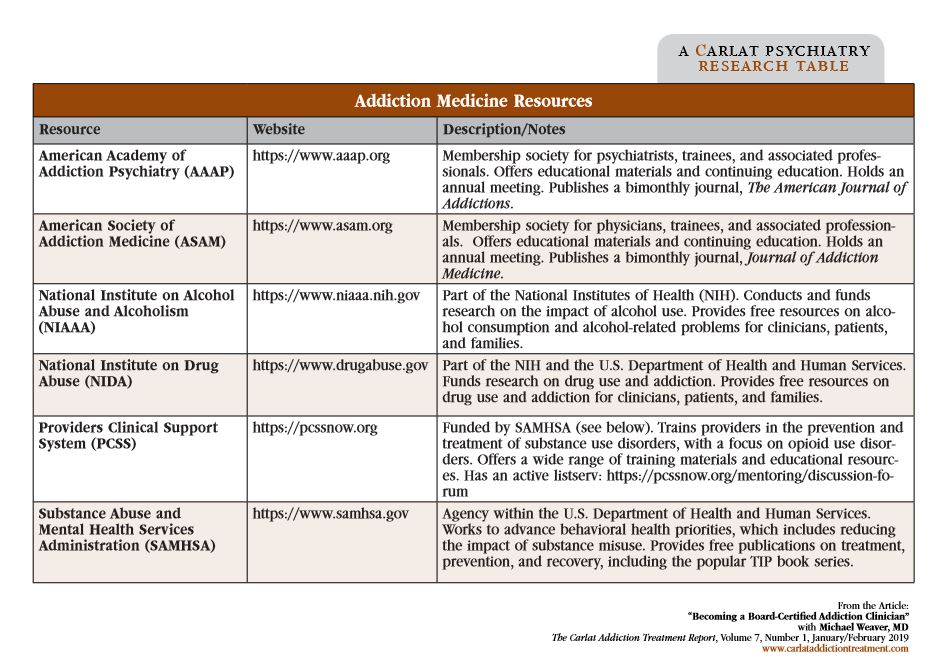
Dr. Weaver: If you’ve met the requirements, then you’re at least doing some addiction practice on a daily or weekly basis, so that in itself would help you just by virtue of having clinical experience. Folks interested in that will likely have sought out CME credits, which is a good way to gain additional knowledge in areas that maybe you don’t see in your individual practice all the time. And because this is a fairly broad specialty, there will be questions about medical as well as psychiatric complications. Being able to consider the breadth of the field is important, and there are a variety of educational opportunities through the American Academy of Addiction Psychiatry (AAAP), the American Society of Addiction Medicine (ASAM), and the Addiction Medicine Foundation. Those last two also have mock self-test programs available that people can utilize in order to get some practice.
CATR: How up-to-date would I have to be on recent advances in the field?
Dr. Weaver: Anything that’s brand-new is probably not going to be tested because the exam covers things that are accepted and practiced in the field. Also, if it’s pretty controversial, it’s probably not going to be tested. The exam covers the basic principles, mainly in the form of clinical scenarios and vignettes that test application of knowledge.
CATR: How often is the exam offered?
Dr. Weaver: Every year. The application period runs from April 1 to June 30, and then the exam itself is in October into November of that year. Applicants are notified of their results in late January of the following year, and that’s when they become board-certified for the standard 10 years.
CATR: Great. Let’s say I took the exam and passed. What does the maintenance of certification (MOC) process look like?
Dr. Weaver: We are still in the process of building it out, but it has the same components that other medical specialties require. So part 1 is just maintaining licensure. Part 2 is lifelong learning—basically CME credits, and ABPM is pretty inclusive in terms of CMEs. So if you are boarded in another primary specialty, then you can have a lot of CMEs counted toward addiction medicine MOC. Part 3 we are working on. Typically, it’s been another high-stakes certification examination. It depends on what ABMS does to change MOC, but it may move like other boards have to more of a longitudinal assessment. And then part 4 is practice improvement modules, and again that’s going to depend on what ABMS does with MOC. We are still in the process of setting that up.
CATR: So folks that have just been certified can start working on parts 1 and 2, and parts 3 and 4 are still in the works.
Dr. Weaver: Yes, for parts 3 and 4 they’ve got a number of years before those become imperative. Another point to add is that for MOC, you are not required to maintain your primary board certification. Board certification in a primary ABMS board is required to apply for initial certification in addiction medicine, but then it is not required to maintain certification in addiction medicine.
CATR: That’s an interesting point. So as a psychiatrist who is board-certified in addiction medicine, I can continue to be certified even if I don’t maintain my psychiatric boards?
Dr. Weaver: Yes, that’s correct. And this works for folks who are not doing general psychiatry anymore. It wouldn’t make sense for them to recertify in general psychiatry if all they are doing is addiction medicine.
CATR: Finally, there is some confusion about the process that the addiction medicine board underwent. It used to be a board administered through ASAM, but now it’s separate?
Dr. Weaver: Right, it used to be an independent board that was not a part of ABMS. Now addiction medicine is under the American Board of Preventive Medicine. That’s the administrating board that said, “We’ll take responsibility for certifying the physicians in the subspecialty of addiction medicine,” but of course, anyone from any other board can apply. Additional details about the board and certification process are on the website at www.theabpm.org.
CATR: Thank you for your time, Dr. Weaver.
Addiction TreatmentDr. Weaver: Patients with addiction are common in psychiatric or any other practice. You’re going to see patients who have these issues, so it’s good to be prepared and able to focus on treating addiction, as well as to be part of a growing group of specialists.
CATR: Are there opportunities that may open up for practitioners as a result of certification?
Dr. Weaver: The opioid crisis has opened the doors to an array of federal funding. And with funding for additional treatment outlets, there are going to be more positions for folks who are knowledgeable about addiction, and certification will eventually become a requirement for that. You can have practice opportunities in a variety of venues, from the more traditional residential focus to the currently popular medication treatment focus. You can also work with other formats such as multilevel specialty programs, freestanding addiction clinics, or even addiction clinics embedded within other practices. Practitioners can also gain recognition as experts in a growing subspecialty and assume leadership positions as administrators, educators, and policy consultants. All of this can open up earning potential.
CATR: There continues to be a tremendous need, and having that certification increases the chances of finding employment in any setting.
Dr. Weaver: Absolutely, and now that addiction medicine is recognized as a subspecialty by the American Board of Medical Specialties (ABMS), it is gaining more credence among medical practitioners. And, of course, addiction psychiatry has been an ABMS subspecialty for quite a while.
CATR: This leads us to an issue that is confusing for many practitioners. Could you tell us about the difference between board certification in addiction psychiatry and addiction medicine?
Dr. Weaver: These are two separate boards. To get certified in addiction psychiatry, you have to be board-certified in psychiatry and complete a 1-year addiction psychiatry fellowship. Addiction medicine is newer and more inclusive—you can come from any specialty, not just psychiatry, and there is no requirement for a fellowship, at least until 2021. Instead, there is a practice pathway, so psychiatrists who have been treating addiction but didn’t do a fellowship may have the opportunity to get board certification by virtue of their clinical practice.
CATR: Are there any differences in focus between addiction psychiatry and addiction medicine?
Dr. Weaver: The differences are pretty minor. Philosophically, addiction medicine may be a little bit broader in terms of addressing more potential medical complications, and may include more aspects of pain management or considerations related to obstetrics. So it may be a little bit more broad-based, but then anyone who has been doing addiction psychiatry for a while probably has encountered some of that in the course of their practice. Addiction psychiatry, on the other hand, has more of a focus on co-occurring psychiatric disorders.
CATR: Makes sense. Let’s talk about the process of board certification in addiction medicine—can you break it down?
Dr. Weaver: Sure. There are a couple of ways to do it, but across all those different pathways to certification in addiction medicine, you need to have certification in a primary board under ABMS. That can be psychiatry, internal medicine, pediatrics, obstetrics—any of those ABMS member boards.
CATR: And then you can do a fellowship or the practice pathway that you mentioned?
Dr. Weaver: Correct. So the fellowship pathway is pretty straightforward. You would do an addiction medicine fellowship. Those are in the process of being accredited by the Accreditation Council for Graduate Medical Education (ACGME), and there are 14 programs currently accredited. You can also complete one that has been accredited by the Addiction Medicine Foundation, formerly known as the American Board of Addiction Medicine and soon to be known as the American College of Academic Addiction Medicine. There are around 50 of those programs, and they also will count, because they basically followed the same guidelines that the ACGME is using.
CATR: Are these 1-year fellowships?
Dr. Weaver: Most of them are. Some institutions have either a requirement or an option for a research-focused 2-year fellowship, so you can do either, but you must do the full fellowship and complete it successfully in order to apply for certification. So if you do a 2-year fellowship, you’ve got to do both years before you apply. If you don’t complete the fellowship, you can count that toward the time in practice, but that would fall under the practice pathway.
CATR: Can you walk us through what the practice pathway is about?
Dr. Weaver: Sure. For the practice pathway, you need to have 1,920 hours of subspecialty-level addiction medicine–specific practice. And those 1,920 hours are basically the equivalent of 1 year’s full-time practice. However, that doesn’t have to be done over 1 year; it can be spread out over the 5 years prior to the time in which you apply for certification. Plus, it requires a minimum of 24 months in practice, so if you did 1 year full-time you wouldn’t meet the requirements; however, if you did 2 years half-time or full-time, then that would meet them. Also, these cannot be hours earned in residency training.
CATR: Do you need to primarily or exclusively treat addiction during these required hours?
Dr. Weaver: Well, you have to be able to describe the kind of addiction-specific practice that you are doing. You can count up to 25% of those 1,920 hours as addiction-specific practice within another primary specialty. For example, if you are doing family medicine and you’re addressing smoking cessation, or you are seeing people and doing motivational interviewing for alcohol use disorder, you can count up to 480 hours if you describe what you are doing consistently in a general practice.
CATR: What about the remaining 75% of the hours?
Dr. Weaver: The other 1,440 hours need to be in addiction medicine–specific practice, but this can include research or teaching. It’s just that 480 of those hours have to be hands-on patient care, so you can’t be doing all academics or all lab. At least 25% has to be hands-on patient care in addiction medicine.
CATR: Could you give us some examples of an addiction-specific practice?
Dr. Weaver: It can take a variety of forms. The simplest example a lot of people think of is prescribing buprenorphine and describing the number of patients and amount of time you spend doing that with patients, and what you do in addition to prescribing in terms of counseling, prevention, and addressing other comorbidities. It could also be spent part-time in a formal treatment facility, such as working as a staff physician or medical director for a residential program doing evaluations for current patients.
CATR: So this would need to be documented in the application. Is there any verification process?
Dr. Weaver: Yes. All of that would need to be verified by someone who is familiar with the individual’s practice—ideally, the direct supervisor, department chair, or chief of staff. But it could also be, for example, another physician in the community who has direct experience through cross-referral of patients, or collegial interactions through medical societies and professional meetings, or someone who works with the applicant who is not under the applicant’s direct supervision.
CATR: So if I were a clinician in private practice who screens every patient for addiction, treats comorbidities, and then treats some addiction directly, would that meet the requirement?
Dr. Weaver: That would count for up to 25% of the 1,920 hours. For the other 1,440 hours, you need to devote time specifically to doing addiction medicine activities separate from that, which could be all those things that I gave examples of earlier. Or you could work in a hospital detox unit or a dual-diagnosis unit, for example.
CATR: So those additional hours would have to be in an addiction specialty setting?
Dr. Weaver: In general, yes. If you’re saying, “Well, I just screen everybody and counsel everybody in my own general practice,” that’s really hard to justify.
CATR: What if I were doing, say, full-time buprenorphine practice in private practice? Would that qualify?
Dr. Weaver: You could say, “Well, here’s the time I set aside for doing that and here’s how many patients I see, and here’s what I do for them.” There’s not a set template for how people are doing these things—obviously there’s some latitude—so it depends on how well people describe what it is that they are doing.
CATR: OK. Let’s say I meet the criteria for the practice pathway and apply for certification. What happens next?
Dr. Weaver: That allows you to sit for the certification exam. The exam is offered at Prometric test centers with the National Board of Medical Examiners. There are about 300 centers in the US, so it’s similar to many other medical certification exams in that respect. It’s a computer-administered secure exam for the initial certification.
CATR: Can you give us some tips on how to prepare for the exam?
Dr. Weaver: If you’ve met the requirements, then you’re at least doing some addiction practice on a daily or weekly basis, so that in itself would help you just by virtue of having clinical experience. Folks interested in that will likely have sought out CME credits, which is a good way to gain additional knowledge in areas that maybe you don’t see in your individual practice all the time. And because this is a fairly broad specialty, there will be questions about medical as well as psychiatric complications. Being able to consider the breadth of the field is important, and there are a variety of educational opportunities through the American Academy of Addiction Psychiatry (AAAP), the American Society of Addiction Medicine (ASAM), and the Addiction Medicine Foundation. Those last two also have mock self-test programs available that people can utilize in order to get some practice.
CATR: How up-to-date would I have to be on recent advances in the field?
Dr. Weaver: Anything that’s brand-new is probably not going to be tested because the exam covers things that are accepted and practiced in the field. Also, if it’s pretty controversial, it’s probably not going to be tested. The exam covers the basic principles, mainly in the form of clinical scenarios and vignettes that test application of knowledge.
CATR: How often is the exam offered?
Dr. Weaver: Every year. The application period runs from April 1 to June 30, and then the exam itself is in October into November of that year. Applicants are notified of their results in late January of the following year, and that’s when they become board-certified for the standard 10 years.
CATR: Great. Let’s say I took the exam and passed. What does the maintenance of certification (MOC) process look like?
Dr. Weaver: We are still in the process of building it out, but it has the same components that other medical specialties require. So part 1 is just maintaining licensure. Part 2 is lifelong learning—basically CME credits, and ABPM is pretty inclusive in terms of CMEs. So if you are boarded in another primary specialty, then you can have a lot of CMEs counted toward addiction medicine MOC. Part 3 we are working on. Typically, it’s been another high-stakes certification examination. It depends on what ABMS does to change MOC, but it may move like other boards have to more of a longitudinal assessment. And then part 4 is practice improvement modules, and again that’s going to depend on what ABMS does with MOC. We are still in the process of setting that up.
CATR: So folks that have just been certified can start working on parts 1 and 2, and parts 3 and 4 are still in the works.
Dr. Weaver: Yes, for parts 3 and 4 they’ve got a number of years before those become imperative. Another point to add is that for MOC, you are not required to maintain your primary board certification. Board certification in a primary ABMS board is required to apply for initial certification in addiction medicine, but then it is not required to maintain certification in addiction medicine.
CATR: That’s an interesting point. So as a psychiatrist who is board-certified in addiction medicine, I can continue to be certified even if I don’t maintain my psychiatric boards?
Dr. Weaver: Yes, that’s correct. And this works for folks who are not doing general psychiatry anymore. It wouldn’t make sense for them to recertify in general psychiatry if all they are doing is addiction medicine.
CATR: Finally, there is some confusion about the process that the addiction medicine board underwent. It used to be a board administered through ASAM, but now it’s separate?
Dr. Weaver: Right, it used to be an independent board that was not a part of ABMS. Now addiction medicine is under the American Board of Preventive Medicine. That’s the administrating board that said, “We’ll take responsibility for certifying the physicians in the subspecialty of addiction medicine,” but of course, anyone from any other board can apply. Additional details about the board and certification process are on the website at www.theabpm.org.
CATR: Thank you for your time, Dr. Weaver.

Issue Date: January 1, 2019
Table Of Contents
Recommended
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2026 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



