Medical Mimics in Geriatric Psychiatry
Miranda Tsang. MD candidate 2024, Tufts University School of Medicine, Boston, MA.
Julia Cromwell, MD. Medical Director, Senior Adult Psychiatry Unit, Salem Hospital, Salem, MA.
Ms. Tsang and Dr. Cromwell have no financial relationships with companies related to this material.
Helen is a 61-year-old woman with bipolar disorder who presents to the emergency department (ED) with altered mental status (AMS). Her family reports that she has been acting increasingly bizarre for weeks, including trying to revive her grandson’s dead pet rabbit and defecating on the floor. She scores a 20/30 on the Montreal Cognitive Assessment (MoCA) but has no history of cognitive impairment. There’s no obvious medical reason for her symptoms, so she’s admitted to inpatient psychiatry for more treatment.
It’s pretty easy to mistake unidentified medical conditions for primary psychiatric disorders, especially since most psychiatric disorders are defined by symptoms without any clear diagnostic test or procedure to confirm the diagnosis. To make things even more complicated, medical conditions can both trigger and worsen psychiatric symptoms. Older adults, especially those with substance use disorders, preexisting medical issues, and no prior psychiatric history, are more likely to have a “medical mimic” (a medical condition closely imitating a primary psychiatric disorder). Failure to identify this condition can lead to delays in proper care and increased health care costs. So how can a psychiatric clinician be more vigilant in spotting these medical mimics? This article gives a quick rundown on how to evaluate and screen for possible medical conditions presenting with psychiatric symptoms.
Checking for medical mimics
A good starting point is to think about delirium in medical inpatients, as well as ED patients and outpatients with AMS. Quick onset of symptoms, fluctuating course, and altered consciousness are key factors suggesting delirium. It’s helpful to get standard screening tests for both new-onset and atypical presentations. Doing a basic mental status exam, physical exam, and neurological exam can also help to spot possible medical mimics that need further evaluation. For example, if your patient has dry mouth, constipation, urinary retention, and blurred vision, think about anticholinergic side effects. Or, if you see twitching and other motor abnormalities, consider hypocalcemia. For more examples of common medical mimics, see table.
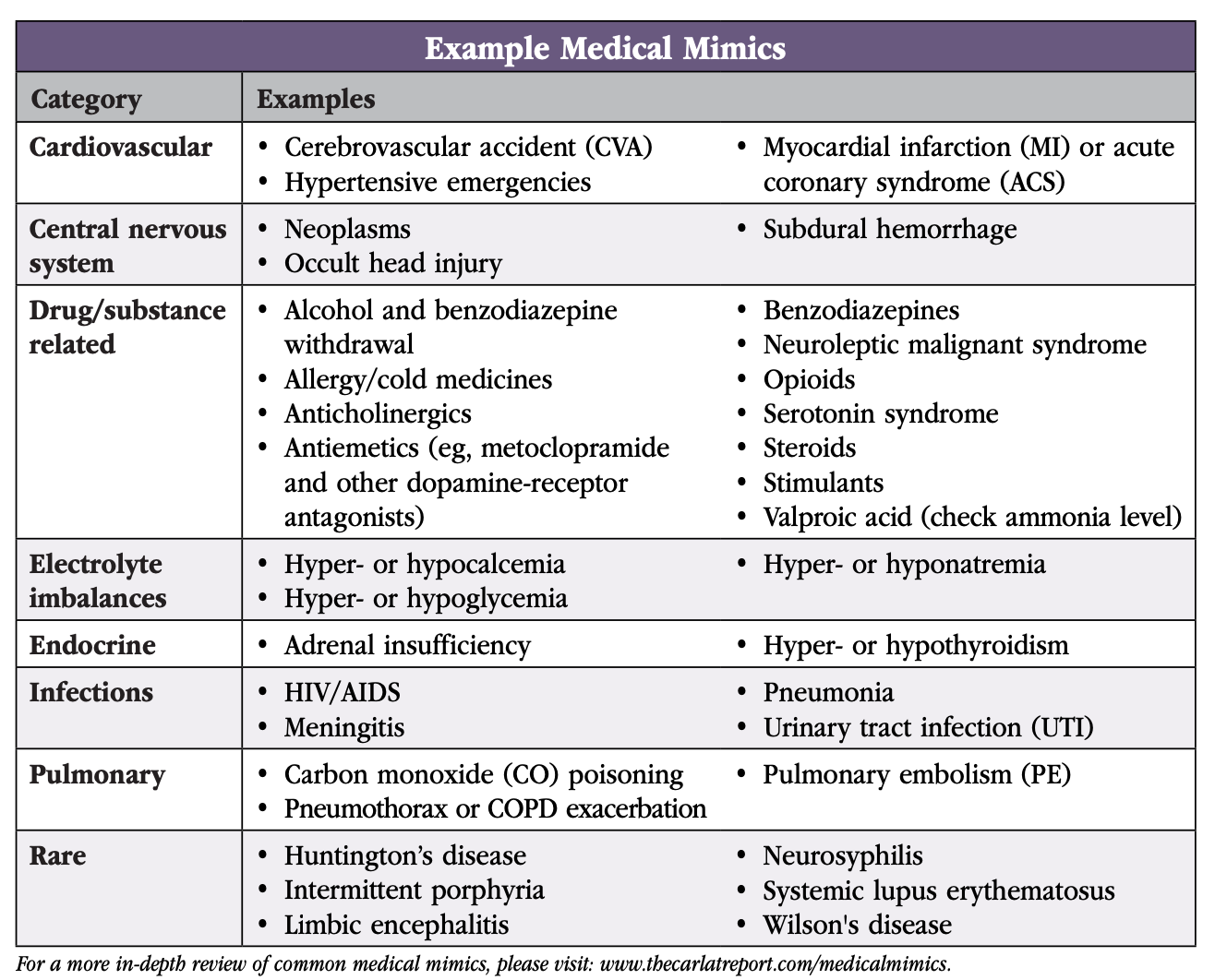 Table. Medical Mimics.
Table. Medical Mimics.
Click to view the PDF
The typical set of screening labs in older adults includes:
- Complete metabolic panel
- Liver function tests
- Complete blood count with differential
- Urine toxicology screen
- Vitamin B12 levels
- Folate levels
- Thyroid panel
- RPR and HIV if high risk
- Urinalysis and chest x-ray (often added in older patients presenting with confusion or respiratory symptoms)
The reasoning behind these labs is to rule out medical causes of delirium or cognitive impairment and to get baseline medical information (Welch KA and Carson AJ, Clin Med (Lond) 2018;18(1):80–87). Not all older adults with confusion need head imaging, but it’s a good idea for those with localizing neurological signs, seizures, significant cognitive impairment not explained by delirium or intoxication, or high risk of falls. Additional workup beyond these basics depends on individual presentations rather than protocols. (See “How to Distinguish the Dementias” article in CGPR Jan/Feb/Mar 2022 for more.)
Before considering a transfer to psychiatry in a patient with AMS, ensure the patient has had an appropriate medical workup based on their symptoms. In practice, you may receive pushback due to clinician bias against mental illness. When you suspect the patient’s psychiatric symptoms have a medical cause, it’s best to communicate your specific concerns and ideas for additional workup. If a medical team is unwilling to evaluate further, consider escalating your concerns to unit leadership.
Example mimics: Respiratory system
Although medical illness affecting almost any organ system can mimic psychiatric illness, the respiratory system deserves special attention. Any difficulty breathing goes hand in hand with anxiety, but some respiratory conditions can be fatal if mistaken for psychiatric illness. Here are a few samples to illustrate example evaluations for conditions you don’t want to miss.
Pneumothorax or COPD exacerbation
Patients with a pneumothorax or COPD exacerbation might present with sudden shortness of breath or pleuritic chest pain, but they might also experience anxiety or confusion. Findings such as tachypnea may be wrongly attributed to hyperventilation from a panic attack. Additional factors that should make you consider further evaluation (eg, a chest x-ray) include:
- Smoking history
- Home oxygen usage
- Changes in sputum production or baseline breathing patterns
Pulmonary embolism
Patients with a pulmonary embolism (PE) might also present with anxiety or a feeling of apprehension or doom. Think about PE especially when anxiety is accompanied by tachycardia, dyspnea, or pleuritic chest pain. The following factors should prompt further workup (eg, a chest CT):
- Hypercoagulable state
- A recent surgery
- Prolonged immobilization
- Trauma
- Cancer
- Family history of PE
Carbon monoxide poisoning
A patient with carbon monoxide (CO) poisoning might present with headache, nausea, dizziness, weakness, and dyspnea, but they could also present with confusion, poor concentration, and irritability. CO poisoning can easily mimic anxiety, depression, or even psychosis. Some patients develop a delayed neuropsychiatric syndrome, characterized by neurological deficits, personality changes, and cognitive problems, weeks after the initial poisoning. Chronic CO poisoning is frequently seen in the winter due to faulty heating systems and poorly ventilated appliances. Common sources include gas heaters, ovens, and wood/gas fires. The yearly incidence of CO poisoning is estimated to be 50,000 (or 16 cases/100,000 population) in the US (Rose JJ et al, Am J Respir Crit Care Med 2017;195(5):596–606). A failure to recognize this diagnosis can be catastrophic.
Back to Helen’s story: On inpatient psychiatry, Helen’s nurse practitioner gets worried after Helen reports headaches and nausea, which have been going on for weeks. She’s transferred back to the medical floor, and an arterial blood gas confirms CO poisoning. She starts hyperbaric oxygen therapy. After a couple weeks of treatment, her bizarre behaviors resolve and her repeat MoCA score improves by 10 points.
CARLAT VERDICT
Medical mimics are not as rare as you might think, especially in the elderly. Learn about the common mimics and get in the habit of judiciously ordering labs so that you don’t miss them.
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2026 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



