New Medications for Insomnia
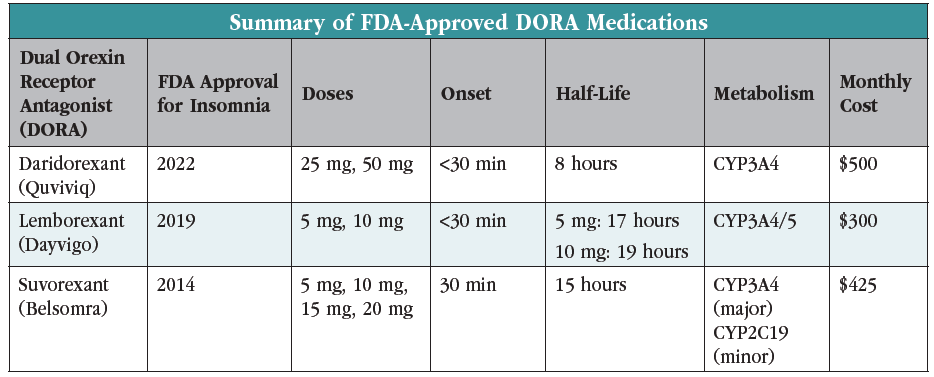
Much of what we do in psychiatry involves helping patients get to sleep, whether they are experiencing depression, anxiety, mania, or just primary insomnia. Over the last several years, we’ve seen the introduction of sleep medications that block orexin receptors. These medications are considered safer than the hypnotics and sedating antidepressants used in the past, but they come with some challenges of their own in practice. In this article, I will review when and how to use the dual orexin receptor antagonist medications (DORAs): daridorexant (Quviviq), lemborexant (Dayvigo), and suvorexant (Belsomra).
How do orexin antagonists work?
Orexin neurons are located primarily in the hypothalamus, an area of the brain known as the “control center” because it regulates the homeostatic balance of many bodily functions, including sleep. High concentrations of orexin receptors in the monoamine centers located in the brainstem are often thought of as “wake-promoting,” but their real function may be to mediate wakefulness by regulating arousal and promoting neurotransmitters such as acetylcholine, dopamine, histamine, norepinephrine, and serotonin. There are two types of orexin receptors—orexin 1 and 2—and the orexin antagonists induce sleep by blocking both receptors.
In narcolepsy, the orexin neurons degenerate, causing sudden sleep attacks throughout the day. Using an orexin antagonist in narcolepsy is absolutely contraindicated because it would cause cataplexy in this population (Muehlan C, J Sleep Res 2023;32(6):e13902).
How well do orexin antagonists work?
Like the Z-hypnotics, orexin antagonists are only FDA approved for primary insomnia. In randomized controlled trials (RCTs), orexin antagonists reduced time to sleep onset, reduced nocturnal awakenings, and increased total sleep time.
Two pivotal randomized placebo-controlled trials resulted in FDA approval for suvorexant. It outperformed placebo on all subjective as well as polysomnography end points in the first week of treatment, at one month, and at three months. Suvorexant was well tolerated, with fewer than 5% of patients discontinuing treatment due to adverse events, and there were no signs of withdrawal symptoms or rebound insomnia when discontinued (Herring WJ et al, Biol Psychiatry 2016;79(2):136–148). Lemborexant shared similar success in a multicenter RCT that showed a decrease from baseline in patient-reported sleep onset, a decrease in waking after sleep onset, and increase in sleep efficiency, in all cases significantly outperforming placebo (Kärppä M et al, Sleep 2020;43(9):szaa123).
The newest DORA is daridorexant, which has a shorter half-life at eight hours, compared to 17–19 hours for lemborexant and 15 hours for suvorexant. In a multicenter RCT, a dose-dependent improvement in reducing waking after sleep onset and sleep latency was observed compared to placebo. Doses of 25 mg and 50 mg improved sleep outcomes, but the 50 mg dose also improved daytime functioning in people with insomnia (Mignot E et al, Lancet Neurol 2022;21(2):125–139). Suvorexant and lemborexant brought similar improvements in daytime functioning.
Although these medications have not been compared head-to-head, indirectly compared in a network meta-analysis. Lemborexant 10 mg had the largest effect size compared to placebo for all primary outcomes, but it had a higher risk of daytime somnolence (Kishi T et al, Psychiatr Res 2020;128:68–74). Despite that risk, the two drugs had similar rates of discontinuation due to adverse effects.
One advantage of the DORAs is their safety record in the elderly population (65 years and older). No new problems stood out in the trials that focused on the elderly, even when the patients were woken in the middle of the night to assess their balance. The DORAs also have a low risk of causing next-day memory problems. Among the hypnotics, only ramelteon has a similar safety profile in the elderly. Trazodone has a reputation as a safe hypnotic, but it carries cardiac risks and can cause falls by causing orthostatic hypotension (Murphy P et al, Clin Sleep Med 2020;16(5):765–773).
In the United States, all DORAs are scheduled in the same class as Z-hypnotics (Schedule IV), indicating a low risk. Animal studies found no evidence of withdrawal and a low risk of reinforcing effects (Born S et al, Regul Toxicol Pharmacol 2017;86:181–192; Schoedel KA et al, J Clin Psychopharmacol 2016;36(4):314–323; Landry I et al, J Clin Psychopharmacol 2022;42(4):365–373). However, studies that tested high doses of DORAs in people with a history of recreational sedative use did find a potential for misuse (Ufer M et al, Sleep 2022;45(3):zsab224). If misuse is a concern, a nonscheduled hypnotic like doxepin or ramelteon is a good alternative.
Adverse effects
The most common adverse effects are dose related and include daytime somnolence and fatigue. Like other hypnotics, the DORAs carry a warning about complex sleep behaviors (eg, sleepwalking, sleep driving), sleep paralysis, hypnagogic/hypnopompic hallucinations, and worsening depression or suicidal ideation. These risks are more strongly associated with the benzodiazepines and Z-hypnotics than the DORAs, but their possibility cannot be ruled out (McCall WV et al, Am J Psychiatry 2017;174(1):18–25). Narcolepsy is the main contraindication to their use.
How to use orexin antagonists
With their safety advantages over the Z-hypnotics and benzodiazepines, the DORAs could be used first line for insomnia, were it not for their cost. Many insurers will require a documented failure of alternative hypnotics before approving them.
The directions for DORAs are similar to other hypnotics: Get into bed after taking the medication and allow for seven hours of sleep before rising. The DORAs begin to take effect within 30 minutes, and that effect is delayed if taken with a large or fatty meal. Daridorexant has the shortest half-life at eight hours, compared to 17–19 hours for lemborexant and 15 hours for suvorexant. All three medications are primarily metabolized by CYP3A4.
Data for transitioning from benzodiazepines or Z-hypnotics are limited, but a small RCT did find that switching from a benzo to suvorexant was effective inpatients whose insomnia was unresponsive to long-term benzodiazepine therapy (Shigetsura Y et al, Clin Neuropharmacol 2022;45(3):52–60). Whether to cross-taper from a benzo or Z-hypnotic is less clear. On the one hand, withdrawal effects may obscure any benefits from the new hypnotic. On the other hand, one study found a significant increase in sedation when suvorexant was added to existing benzodiazepine treatment (Hatano M et al, Clin Psychopharmacol Neurosci 2018;16(2):184–189).
CARLAT VERDICT
DORAs fill a much-needed gap in insomnia research. They offer an enhanced safety profile with decreased risk for withdrawal and dependence, but cost and lack of evidence in psychiatric disorders other than primary insomnia remain barriers to widespread clinical use.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



