Navigating Ethical Challenges in Geriatric Psychiatry

There are specific ethical challenges that clinicians working with older adults are likely to encounter. These range from assessing a patient’s capacity to live independently or drive safely to identifying elder abuse. This article explores the unique domains of capacity evaluation within geriatric psychiatry, while also shedding light on the pressing topics of elder abuse and advance health care planning.
Capacity for independent living
It’s essential to thoroughly assess the level of support older adults require to maintain their well-being and safety. This assessment covers five domains, each playing a key role in determining their overall care needs:
- Personal needs and hygiene: Can the patient handle the basics (eg, bathing, dressing)?
- Home environment: Is their living space safe and appropriate?
- Activities like shopping, meal planning, and transportation: How well can they manage shopping and cooking? Can they get around safely?
- Illness and medication management: Are they on top of their health and medications?
- Financial management: Can they handle their money appropriately?
(Source: Skelton F et al, Arch Gerontol Geriatr 2010;50(3):300–305)
We will delve into the assessments of driving capacity and financial management capacity in their own sections, as these topics tend to come up frequently in clinical discussions.
In these evaluations, focus on decisional and executive capacities.
Decisional capacity
When evaluating decisional capacity, you are trying to figure out how well your patients understand and express their preferences and limitations. It’s not just about what they choose, but how they communicate these choices. (For more on assessing decisional capacity, see our Q&A on “Ethical Principles and Capacity Assessment in Dementia Care.”)
Executive capacity
Here, you’re evaluating whether your patients can actually accomplish what they need to accomplish. I recommend the “articulate-demonstrate” method, which is a practical approach that I’ve found works well with many patients (Naik AD et al, Geriatrics 2008;63(2):24–31). For instance, when assessing your patient’s capacity to manage their medications, find out whether they can tell you what they should be taking (ie, can they articulate this knowledge) and whether they can manage the pillbox and coordinate with the pharmacy (ie, can they demonstrate this skill).
Comprehensive evaluations
Sometimes, you need a more comprehensive evaluation than you have the time or the skills to conduct. In these cases, I recommend considering a referral to occupational therapy. Occupational therapists often use validated tools like the Kohlman Evaluation of Living Skills to assess abilities related to activities of daily living. You may also consider referral for a social work assessment or physical therapy evaluation.
Capacity to drive safely
To evaluate an older adult’s driving safety:
- Ask how often the patient drives and whether they have had any recent accidents, incidents, or near misses
- Ask caregivers about their observations, but keep in mind they often underestimate a patient’s decline in driving skills
- Consider how the patient’s health and medications might impact their driving
(Source: Balasubramaniam M et al, eds. Psychiatric Ethics in Late-Life Patients: Medicolegal and Forensic Aspects at the Interface of Mental Health. Cham, Switzerland: Springer; 2019)
I usually ask families about the age of the youngest child in the household. I then ask if they’d be at ease having that child ride solo in a car with the patient behind the wheel. I’ve noticed that even families who initially give the patient a thumbs-up for driving often change their tune and say “no” to the second question. That’s when I dig more and ask for additional details. I also pay special attention to cognitive assessment results, like difficulties with clock drawing or the Trail Making Test, as these can be red flags for impaired driving. (For more, see CGPR Oct/Nov/Dec 2023.)
When in doubt, I recommend reporting your concerns to the Department of Motor Vehicles. A report typically triggers a road test but does not automatically suspend driving privileges. Don’t forget to acknowledge the emotional toll on your patient when discussing the loss of driving privileges. For many older adults, driving is not just about getting from A to B; it symbolizes independence and control.
Capacity to manage finances
Bring up discussions about financial capacity early in the course of cognitive disorders. Educate caregivers on how to spot signs of financial impairment (eg, missed bills, duplicate payments, overlooked tax deadlines, unusual transactions in bank accounts, questionable investments, and unexpected donations).
When assessing financial capacity, focus on two things:
- Performance: Can the patient execute tasks (eg, paying bills, managing accounts)?
- Judgment: Are they able to understand consequences and risks and make sound financial decisions?
Ask for specifics. You want to make sure patients have the skills to handle their finances independently and safely in their current setup. For instance, a patient who handles bills solo and dives into the stock market needs a higher skill level than someone with a cognitively intact spouse taking charge of the finances.
Assessing your patient’s judgment is especially relevant in patients with suspected frontotemporal dementia, as their decline in judgment tends to happen earlier and be more profound than their decline in ability to perform tasks.
Sometimes, patients are hesitant to hand over financial control even when others are worried about their ability to manage their finances. In these cases, I suggest teaming up with the patient’s bank to set up safeguards, like overdraft protection, joint account holders, or authorized signers. When faced with more complex questions, such as those involving testamentary capacity, I recommend involving neuropsychologists or forensic psychologists (Marson D, Public Policy Aging Rep 2016;26(1):12–14). I also refer patients to elder law attorneys to assist with wills, estate planning, and the appointment of a durable power of attorney.
Identifying and reporting elder abuse
Elder abuse is sadly common, affecting approximately one in 10 older adults in the US (Lachs MA and Pillemer KA, New Engl J Med 2015;373(20):1947–1956). It can show up in different ways like physical or emotional abuse, financial exploitation, or neglect. When evaluating for elder abuse:
- First cover the basics (eg, food and medicines)
- Ask about specific issues (eg, verbal outbursts, signing unfamiliar forms)
- Make use of evaluation tools, such as the Elder Abuse Suspicion Scale, for a structured assessment that covers different types of abuse and neglect (Yaffe MJ et al, J Elder Abuse Negl 2008;20(3):276–300)
Look out for both spoken and unspoken signals from the patient—fear, withdrawal, or anxiety should make you suspicious. Also, watch for physical signs, including the following:
- Fractures in atypical locations
- Traumatic alopecia
- Malnourishment
- Poorly managed health conditions
- Anorectal or vaginal bleeding
If there are urgent medical concerns, consider hospitalization.
In most states, health care workers are required to report elder abuse to Adult Protective Services (APS) or other relevant authorities. The rules may vary, so be sure to check your state’s APS guidelines (www.tinyurl.com/2m44c2fp). When in doubt, err on the side of reporting.
Advance health care planning
It’s a good idea to start discussions about advance health care planning when the patient is doing well. Make it an ongoing conversation, not just a one-time event. As health and situations shift, so can preferences. I always include loved ones in these discussions.
Advance health care planning is formalized into legal documents known as advance directives. There are two main types: living will and power of attorney.
Living will
- A document outlining the patient’s treatment preferences, particularly as they approach the end of life
- Addresses medical conditions and interventions (eg, resuscitation, intubation, tube feeding, dialysis, medication preferences, organ and tissue donation)
- May specify the patient’s palliative care desires and preferred place of death
Power of attorney
- A legal instrument delegating decision-making authority to another person on behalf of the patient
- The extent of authority may vary, covering either specific or comprehensive responsibilities
Actively inform and advocate for the designation of a durable power of attorney. Unlike a standard power of attorney, which becomes invalid when a person becomes mentally incapacitated, a durable power of attorney maintains its validity, and the designated person can continue to make decisions on the patient’s behalf.
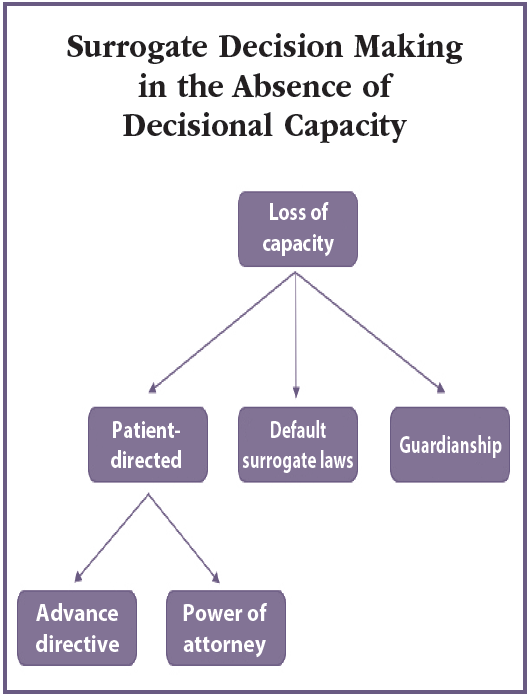
When a patient can’t make decisions and has not left any guidance, most states have a hierarchy for surrogate decision making. It typically begins with the spouse (unless legally separated), followed by an adult child, parent, and adult siblings (see “Surrogate Decision Making in the Absence of Decisional Capacity” figure). Each state has its own rules for settling disputes among surrogates. If there’s no advance directive or suitable surrogates, the legal system might appoint a guardian or conservator. However, it’s wise to consider guardianship as a last resort due to potential drawbacks, including loss of privacy and autonomy, legal costs, and the chance of hasty institutionalization.
CARLAT VERDICT
Familiarize yourself with the steps to assess an elderly patient's capacity in areas like driving, independent living, and financial management. Stay vigilant for signs that elderly patients might be at risk of neglect or abuse, and make sure to report any suspicions of mistreatment promptly to APS. Additionally, integrate routine conversations about advance health care planning into your interactions with patients.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



