Home » Light and Darkness in Bipolar Disorder
EXPERT Q&A
Light and Darkness in Bipolar Disorder
February 1, 2019
From The Carlat Psychiatry Report
 Jim Phelps, MD
Jim Phelps, MD
Psychiatrist and author, Corvallis, OR. Creator, psycheducation.org Dr. Phelps has disclosed that he has no relevant financial or other interests in any commercial companies pertaining to this educational activity.
Dr. Jim Phelps is the author of a textbook on bipolar spectrum disorders, A Spectrum Approach to Mood Disorders: Not Fully Bipolar But Not Unipolar—Practical Management (W. W. Norton & Company) as well as two self-help books on bipolar disorder. He conducted some of the early studies on dark therapy out of his private practice in Oregon, and we caught up with him to learn about this novel treatment for bipolar disorder.
TCPR: You helped develop a treatment for bipolar disorder that’s getting a lot of attention lately. Tell us about this “dark therapy.”
Dr. Phelps: People with mood disorders have problems with their circadian rhythm, and regular exposure to light and darkness helps stabilize that rhythm. Timing is key here. Morning darkness can cause depression, and evening light can trigger mania. In dark therapy, people get into darkness in the early evening and stay overnight in a pitch-dark room. So it’s kind of the converse of light therapy, where people sit under a bright light in the morning. Light therapy is well-established for depression, and there is new research suggesting that dark therapy is very effective in bipolar mania.
TCPR: Where did dark therapy come from?
Dr. Phelps: The idea goes back to the 1990s. Tom Wehr and his colleagues at the National Institute of Mental Health (NIMH) had shown that people sleep better when they’re kept in pitch darkness from 6:00 pm to 8:00 am. Now, they knew that insomnia could cause mania, so they tried this dark-room idea in a patient who had intractable rapid cycling. With his consent, they put the patient in a pitch-dark room overnight, from 6:00 pm to 8:00 am. He quickly went from experiencing weekly cycles of mania and depression to a full recovery (Wehr TA et al, Biol Psychiatry 1998;43(11):822–828).
TCPR: That’s an impressive case. What has the research shown since then?
Dr. Phelps: Next, there was a small controlled trial in hospitalized manic patients. It was only positive in patients whose manias had lasted less than 2 weeks, so we couldn’t really conclude that dark therapy worked at that point (Barbini B et al, Bipolar Disord 2005;7(1):98–101). Fast forward to 2016, and the first randomized, placebo-controlled trial came out, again in hospitalized mania. The improvements were dramatic over the first week, with a large effect size of 1.9, while the control group barely changed (Henriksen TE et al, Bipolar Disord 2016;18(3):221–232).
TCPR: Were there any flaws in that study?
Dr. Phelps: Well, it’s just one study, and it was a small one (24 subjects). My opinion, though, is that a treatment that’s inexpensive and low-risk ought to have a lower bar of entry for clinical use. The findings still need replication, but if this were a medication that could cause diabetes or raise cholesterol, I’d want to see a lot more confirmation before using it.
TCPR: What about blinding? Didn’t the patients know they were getting dark therapy?
Dr. Phelps: That’s where it gets interesting. This study used a new type of dark therapy with special glasses that create “virtual darkness.” The glasses have an amber tint, and the control group wore glasses with a grayish tint, so the patients couldn’t tell which treatment they were receiving. It was the raters who weren’t completely blinded. To rate manic symptoms in a 24-hour period, they incorporated input from the hospital staff, and those staff knew what the amber-colored glasses meant. There was one blinded assessment, though: actigraphy. Mania is a hyperactive state, so wrist actigraphy is increasingly used to measure it. The dark therapy group had a significant drop in their overactivity.
TCPR: Tell us more about these amber glasses.
Dr. Phelps: There’s a story there, and it also begins in the 1990s: with the discovery of melanopsin. This is a photoreceptor in the eye, but instead of connecting to the visual cortex, melanopsin connects to the suprachiasmatic nucleus, which regulates the biologic clock. Its whole purpose is to tell the brain whether it’s light or dark outside. And here’s the twist—melanopsin only responds to blue light, so if we block that wavelength, the brain will think it’s in pitch darkness. Eliminating blue light triggers changes in the brain that set the stage for sleep, like raising melatonin.
TCPR: How do you eliminate blue light?
Dr. Phelps: That’s what the amber glasses do. Around 15 years ago, I came across this research and wondered if there was a way to create dark therapy by eliminating blue light. It turns out that evening blue light is linked to other health problems, like breast cancer. There’s a company, www.LowBlueLights.com, that makes amber-tinted glasses that block blue light for medical purposes. They graciously gave me many pairs to try out in a series of bipolar patients in my private practice. (Editor’s note: Dr. Phelps does not have financial interests in specific products.)
TCPR: What did you find?
Dr. Phelps: These were outpatients, and they were relatively stable, with some hypomania, mixed states, and a lot of insomnia going on. About half of them came back and said, “Wow, when I wear these for a couple of hours before bed, I sleep better. I go to sleep sooner, like an hour sooner.” They were really impressed. The other 50% said, “Nah, interesting idea, but these don’t do anything” (Phelps J, Med Hypotheses 2008;70(2):224–229).
TCPR: Walk us through dark therapy.
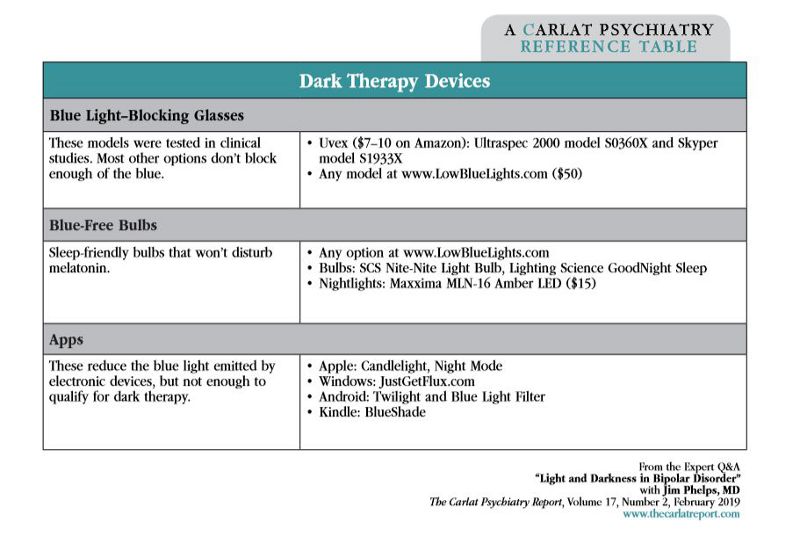
Dr. Phelps: Basically, patients have to be in real darkness or virtual darkness overnight. There are three ways to do this. They can be in a pitch-dark room, or if the lights are on they can wear blue light–blocking glasses. Patients can also use special blue-free light bulbs, as long as the room is otherwise pitch-dark. These are lights that don’t emit any blue wavelengths; they emit a sort of yellow-colored light. There are also ways to reduce blue light in devices, through special settings or apps, but they don’t completely eliminate the blue light. Those may be good for general health, but they’re not going to cut it for dark therapy (see “Dark Therapy Devices” table).
TCPR: What about the timing?
Dr. Phelps: For full mania, the dark protocol extends from 6:00 pm to 8:00 am. That’s hard for patients to stick to, so I’ll involve family or friends if they’re not in the hospital. Once the patient recovers, the darkness can start at a later time, like 8:00 pm to 10:00 pm. In my experience, you can start at that later time in mild cases, and adherence is a lot better when patients don’t have to wear the glasses so early in the evening.
TCPR: Do you ever start earlier than 6:00 pm?
Dr. Phelps: No. That could worsen mood by disrupting the circadian rhythm. It’s worth warning patients about this. Some find the blue-light blockers calming and start wearing them all day long.
TCPR: Are there any side effects?
Dr. Phelps: Possibly depression. In the hospital study, 2 patients developed depression with the amber lenses. It remitted when the lenses were either delayed from 6:00 pm to later in the evening or just stopped entirely. I’ve seen that in my own practice, but then again I’ve seen that with just about any anti-manic therapy when it’s given too aggressively. Headaches have also been reported.
TCPR: How does the world look through these glasses?
Dr. Phelps: It’s still bright, but everything has a warm, yellow glow. Think fireside, starlight, candlelight—that’s the type of light our species evolved under at night for thousands of years. It’s only been in the past century, and more so the past decade, that blue light has made its way into the evening hours. Smartphones, LED screens, TVs, and energy-efficient bulbs are the main sources. Those smartphones may be small, but when you hold them close to your face, it can suppress melatonin as much as a large-screen TV that’s on the other side of the room.
TCPR: Are people with bipolar disorder the only ones affected by this?
Dr. Phelps: No, but they have to be more careful than the rest of us because anything that disrupts sleep can set off new episodes. They’re not completely alone, though, as nocturnal light takes a toll on general health. It worsens concentration the next day, and raises the risk of breast cancer, obesity, heart disease, and diabetes. It’s also linked to depression. In the largest study, sleeping with a dim light in the bedroom, like a nightlight, nearly doubled the risk of depression over 2 years. It wasn’t a controlled study, but the animal data on this are so strong that controlled studies of nocturnal light are considered to be unethical in humans (Obayashi K et al, Am J Epidemiol 2018;187:427–434).
TCPR: How do your patients get their rooms pitch-dark?
Dr. Phelps: I begin by asking, “How much light is there in your bedroom?” Lots of people live near a street light, and blackout curtains can help with that. Some of my patients use tinfoil on the inside of the window. An eye mask can help if they’re not able to get the room dark enough.
TCPR: What about television in the bedroom?
Dr. Phelps: That’s a tough one. People with depression don’t like to lie in the dark with their own thoughts, so they will do things in order to avoid that. Often they will stay awake with lighting devices, such as televisions or screens of various kinds, which then delays their sleep. For many patients, a pair of earbuds with music, radio, or podcasts will have the same effect. UCLA’s Center for Meditative Studies has free programs that are very good for helping to calm the mind (www.uclahealth.org/marc/audio).
TCPR: Can blue-light blockers help insomnia?
Dr. Phelps: The studies are small, but reducing blue light seems to deepen sleep and help people fall asleep earlier. However, they don’t have a sedative effect, so you have to manage expectations in an insomniac who may be hoping to be knocked out by them. I recommend patients with insomnia wear them 1 to 2 hours before bed (Shechter A et al, J Psychiatr Res 2018;96:196–202).
TCPR: What about in depression?
Dr. Phelps: They might help there, but the studies are small and the results have been mixed. There was a positive study in postpartum depression, where the women wore blue-light blockers when they got up to nurse their child (Bennett S et al, Med Hypotheses 2009;73:251–253). The negative trial was in depressed patients with insomnia, but the glasses they used were uncomfortable, so compliance was a big issue (Esaki Y et al, Chronobiol Int 2017;34(6):753–761). What I recommend for depression is morning light.
TCPR: I imagine that’s hard to get with blackout curtains on.
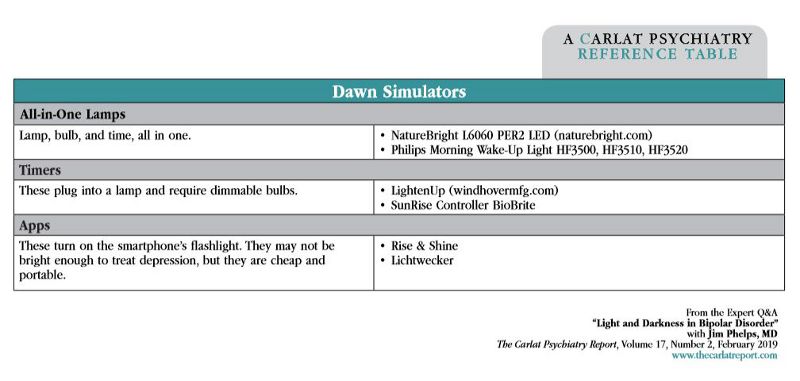
Dr. Phelps: Yes, and morning light is also dim in the wintertime and for anyone living north of the 30th–40th latitude, which is most of the U.S. above Texas or Georgia. This is where dawn simulators are helpful. They create a virtual sunrise in the bedroom, and they’ve worked for winter depression in a handful of small, controlled studies. They aren’t as powerful as a lightbox, but they are risk-free, low-cost, and easy to use. My standard recommendation is LightenUp, which makes affordable models for $15 to $30 (see “Dawn Simulators” table).
TCPR: Can they be used with dark therapy?
Dr. Phelps: Yes. They have no risk of causing mania. Patients program the device for the time they want to wake up. It then turns on gradually in the 30 to 60 minutes before the specified wake-up time. People tend to feel more alert when they wake up to these because it lifts them gradually out of deep sleep. By turning on at the same time each day, a dawn simulator can help keep the circadian rhythm in line.
TCPR: How important is regular timing in bipolar disorder?
Dr. Phelps: Very important. I see dark therapy and light therapy as part of a broader approach to bipolar disorder that involves regulating circadian rhythms. That’s the goal of social rhythm therapy (SRT), a psychotherapy with good evidence in bipolar. SRT helps patients identify and regulate key events that help set their circadian rhythm and stabilize their mood. Light and darkness are important, but so are physical activity, meal times, and contact with people. It’s the timing of these things that matters in bipolar disorder.
TCPR: Thank you for your time, Dr. Phelps.
General Psychiatry Expert Q&ATCPR: You helped develop a treatment for bipolar disorder that’s getting a lot of attention lately. Tell us about this “dark therapy.”
Dr. Phelps: People with mood disorders have problems with their circadian rhythm, and regular exposure to light and darkness helps stabilize that rhythm. Timing is key here. Morning darkness can cause depression, and evening light can trigger mania. In dark therapy, people get into darkness in the early evening and stay overnight in a pitch-dark room. So it’s kind of the converse of light therapy, where people sit under a bright light in the morning. Light therapy is well-established for depression, and there is new research suggesting that dark therapy is very effective in bipolar mania.
TCPR: Where did dark therapy come from?
Dr. Phelps: The idea goes back to the 1990s. Tom Wehr and his colleagues at the National Institute of Mental Health (NIMH) had shown that people sleep better when they’re kept in pitch darkness from 6:00 pm to 8:00 am. Now, they knew that insomnia could cause mania, so they tried this dark-room idea in a patient who had intractable rapid cycling. With his consent, they put the patient in a pitch-dark room overnight, from 6:00 pm to 8:00 am. He quickly went from experiencing weekly cycles of mania and depression to a full recovery (Wehr TA et al, Biol Psychiatry 1998;43(11):822–828).
TCPR: That’s an impressive case. What has the research shown since then?
Dr. Phelps: Next, there was a small controlled trial in hospitalized manic patients. It was only positive in patients whose manias had lasted less than 2 weeks, so we couldn’t really conclude that dark therapy worked at that point (Barbini B et al, Bipolar Disord 2005;7(1):98–101). Fast forward to 2016, and the first randomized, placebo-controlled trial came out, again in hospitalized mania. The improvements were dramatic over the first week, with a large effect size of 1.9, while the control group barely changed (Henriksen TE et al, Bipolar Disord 2016;18(3):221–232).
TCPR: Were there any flaws in that study?
Dr. Phelps: Well, it’s just one study, and it was a small one (24 subjects). My opinion, though, is that a treatment that’s inexpensive and low-risk ought to have a lower bar of entry for clinical use. The findings still need replication, but if this were a medication that could cause diabetes or raise cholesterol, I’d want to see a lot more confirmation before using it.
TCPR: What about blinding? Didn’t the patients know they were getting dark therapy?
Dr. Phelps: That’s where it gets interesting. This study used a new type of dark therapy with special glasses that create “virtual darkness.” The glasses have an amber tint, and the control group wore glasses with a grayish tint, so the patients couldn’t tell which treatment they were receiving. It was the raters who weren’t completely blinded. To rate manic symptoms in a 24-hour period, they incorporated input from the hospital staff, and those staff knew what the amber-colored glasses meant. There was one blinded assessment, though: actigraphy. Mania is a hyperactive state, so wrist actigraphy is increasingly used to measure it. The dark therapy group had a significant drop in their overactivity.
TCPR: Tell us more about these amber glasses.
Dr. Phelps: There’s a story there, and it also begins in the 1990s: with the discovery of melanopsin. This is a photoreceptor in the eye, but instead of connecting to the visual cortex, melanopsin connects to the suprachiasmatic nucleus, which regulates the biologic clock. Its whole purpose is to tell the brain whether it’s light or dark outside. And here’s the twist—melanopsin only responds to blue light, so if we block that wavelength, the brain will think it’s in pitch darkness. Eliminating blue light triggers changes in the brain that set the stage for sleep, like raising melatonin.
TCPR: How do you eliminate blue light?
Dr. Phelps: That’s what the amber glasses do. Around 15 years ago, I came across this research and wondered if there was a way to create dark therapy by eliminating blue light. It turns out that evening blue light is linked to other health problems, like breast cancer. There’s a company, www.LowBlueLights.com, that makes amber-tinted glasses that block blue light for medical purposes. They graciously gave me many pairs to try out in a series of bipolar patients in my private practice. (Editor’s note: Dr. Phelps does not have financial interests in specific products.)
TCPR: What did you find?
Dr. Phelps: These were outpatients, and they were relatively stable, with some hypomania, mixed states, and a lot of insomnia going on. About half of them came back and said, “Wow, when I wear these for a couple of hours before bed, I sleep better. I go to sleep sooner, like an hour sooner.” They were really impressed. The other 50% said, “Nah, interesting idea, but these don’t do anything” (Phelps J, Med Hypotheses 2008;70(2):224–229).
TCPR: Walk us through dark therapy.
Dr. Phelps: Basically, patients have to be in real darkness or virtual darkness overnight. There are three ways to do this. They can be in a pitch-dark room, or if the lights are on they can wear blue light–blocking glasses. Patients can also use special blue-free light bulbs, as long as the room is otherwise pitch-dark. These are lights that don’t emit any blue wavelengths; they emit a sort of yellow-colored light. There are also ways to reduce blue light in devices, through special settings or apps, but they don’t completely eliminate the blue light. Those may be good for general health, but they’re not going to cut it for dark therapy (see “Dark Therapy Devices” table).
TCPR: What about the timing?
Dr. Phelps: For full mania, the dark protocol extends from 6:00 pm to 8:00 am. That’s hard for patients to stick to, so I’ll involve family or friends if they’re not in the hospital. Once the patient recovers, the darkness can start at a later time, like 8:00 pm to 10:00 pm. In my experience, you can start at that later time in mild cases, and adherence is a lot better when patients don’t have to wear the glasses so early in the evening.
TCPR: Do you ever start earlier than 6:00 pm?
Dr. Phelps: No. That could worsen mood by disrupting the circadian rhythm. It’s worth warning patients about this. Some find the blue-light blockers calming and start wearing them all day long.
TCPR: Are there any side effects?
Dr. Phelps: Possibly depression. In the hospital study, 2 patients developed depression with the amber lenses. It remitted when the lenses were either delayed from 6:00 pm to later in the evening or just stopped entirely. I’ve seen that in my own practice, but then again I’ve seen that with just about any anti-manic therapy when it’s given too aggressively. Headaches have also been reported.
TCPR: How does the world look through these glasses?
Dr. Phelps: It’s still bright, but everything has a warm, yellow glow. Think fireside, starlight, candlelight—that’s the type of light our species evolved under at night for thousands of years. It’s only been in the past century, and more so the past decade, that blue light has made its way into the evening hours. Smartphones, LED screens, TVs, and energy-efficient bulbs are the main sources. Those smartphones may be small, but when you hold them close to your face, it can suppress melatonin as much as a large-screen TV that’s on the other side of the room.
TCPR: Are people with bipolar disorder the only ones affected by this?
Dr. Phelps: No, but they have to be more careful than the rest of us because anything that disrupts sleep can set off new episodes. They’re not completely alone, though, as nocturnal light takes a toll on general health. It worsens concentration the next day, and raises the risk of breast cancer, obesity, heart disease, and diabetes. It’s also linked to depression. In the largest study, sleeping with a dim light in the bedroom, like a nightlight, nearly doubled the risk of depression over 2 years. It wasn’t a controlled study, but the animal data on this are so strong that controlled studies of nocturnal light are considered to be unethical in humans (Obayashi K et al, Am J Epidemiol 2018;187:427–434).
TCPR: How do your patients get their rooms pitch-dark?
Dr. Phelps: I begin by asking, “How much light is there in your bedroom?” Lots of people live near a street light, and blackout curtains can help with that. Some of my patients use tinfoil on the inside of the window. An eye mask can help if they’re not able to get the room dark enough.
TCPR: What about television in the bedroom?
Dr. Phelps: That’s a tough one. People with depression don’t like to lie in the dark with their own thoughts, so they will do things in order to avoid that. Often they will stay awake with lighting devices, such as televisions or screens of various kinds, which then delays their sleep. For many patients, a pair of earbuds with music, radio, or podcasts will have the same effect. UCLA’s Center for Meditative Studies has free programs that are very good for helping to calm the mind (www.uclahealth.org/marc/audio).
TCPR: Can blue-light blockers help insomnia?
Dr. Phelps: The studies are small, but reducing blue light seems to deepen sleep and help people fall asleep earlier. However, they don’t have a sedative effect, so you have to manage expectations in an insomniac who may be hoping to be knocked out by them. I recommend patients with insomnia wear them 1 to 2 hours before bed (Shechter A et al, J Psychiatr Res 2018;96:196–202).
TCPR: What about in depression?
Dr. Phelps: They might help there, but the studies are small and the results have been mixed. There was a positive study in postpartum depression, where the women wore blue-light blockers when they got up to nurse their child (Bennett S et al, Med Hypotheses 2009;73:251–253). The negative trial was in depressed patients with insomnia, but the glasses they used were uncomfortable, so compliance was a big issue (Esaki Y et al, Chronobiol Int 2017;34(6):753–761). What I recommend for depression is morning light.
TCPR: I imagine that’s hard to get with blackout curtains on.
Dr. Phelps: Yes, and morning light is also dim in the wintertime and for anyone living north of the 30th–40th latitude, which is most of the U.S. above Texas or Georgia. This is where dawn simulators are helpful. They create a virtual sunrise in the bedroom, and they’ve worked for winter depression in a handful of small, controlled studies. They aren’t as powerful as a lightbox, but they are risk-free, low-cost, and easy to use. My standard recommendation is LightenUp, which makes affordable models for $15 to $30 (see “Dawn Simulators” table).
TCPR: Can they be used with dark therapy?
Dr. Phelps: Yes. They have no risk of causing mania. Patients program the device for the time they want to wake up. It then turns on gradually in the 30 to 60 minutes before the specified wake-up time. People tend to feel more alert when they wake up to these because it lifts them gradually out of deep sleep. By turning on at the same time each day, a dawn simulator can help keep the circadian rhythm in line.
TCPR: How important is regular timing in bipolar disorder?
Dr. Phelps: Very important. I see dark therapy and light therapy as part of a broader approach to bipolar disorder that involves regulating circadian rhythms. That’s the goal of social rhythm therapy (SRT), a psychotherapy with good evidence in bipolar. SRT helps patients identify and regulate key events that help set their circadian rhythm and stabilize their mood. Light and darkness are important, but so are physical activity, meal times, and contact with people. It’s the timing of these things that matters in bipolar disorder.
TCPR: Thank you for your time, Dr. Phelps.
KEYWORDS bipolar mood disorders

Issue Date: February 1, 2019
Table Of Contents
Recommended
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2026 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



