How to Write an Open Note
“A physician should at all times deal honestly and openly with patients.” —AMA Code of Medical Ethics
Beginning April 4, 2021, the Department of Health and Human Services (DHHS) instituted a new policy stating that all clinical notes must be open to patients for their review in a timely fashion. Since that announcement, I have heard physician colleagues from various specialties voice concerns over what this means for us, our patients, and the future of our field. In this article, we’ll take a close look at this new regulation and how it might affect our clinical practices.
The new rules
The new rules are part of the 21st Century Cures Act, which aims to modernize various aspects of medicine, from clinical trials to electronic health records (EHRs). The intent of the ruling is to remove obstacles to patient records so they can be viewed by patients and shared more easily across health care systems. The mandate is handed down by Medicare, Medicaid, and DHHS.
The first part of the ruling applies mainly to developers of EHRs. It requires them to adopt a standardized interface so that electronic records can be shared across platforms. This will take time, and the ruling allows developers 3 years to prepare this rollout.
The second part is the open notes provision, which pertains more directly to clinicians. Under this provision, clinicians must allow patients full access to their medical information without charge or delay. The information must be available to patients through an electronic portal so that they can read it without having requested it.
The exact time frame of a “delay” is not defined, but DHHS does give an example that gets the point across. If a practice withholds labs from a patient to allow their physician time to review and comment on the results, that would be considered a delay.
There are four exceptions to this transparency rule, and I’d suggest clinicians treat them as rarities, not goals.
- Serious imminent harm. Clinicians can withhold records if releasing them could cause imminent harm to the patient or others. However, the ruling states that “emotional damage” does not qualify as harm, and it allows patients the right to an independent review of this exclusion.
- Psychotherapy process notes. Since the early days of HIPAA, therapists have been allowed to keep private psychotherapy process notes separate from the medical record. The new ruling still allows this, but it specifies that medical information pertaining to symptoms and diagnoses cannot be cloistered in a psychotherapy note.
- Legal notes. Information that is “compiled in reasonable anticipation of, or for use in, a civil, criminal, or administrative action or proceeding,” can be withheld, such as communications with a lawyer around a malpractice suit or documentation pertaining to a civil commitment hearing.
- Off the grid. Clinicians who do not use an EHR are exempt from this legislation for now.
Next I’ll look at ways that open notes can improve the physician-patient relationship.
From HIPAA to open notes
While the new ruling expands patient access to the medical record, it is not the first to open up the notes. That started with HIPAA, which broke new ground in the 1990s by requiring medical providers to release notes to patients upon request, unless releasing them could potentially be harmful. The problem was that “harm” was never defined, and some providers interpreted it broadly in a way that precluded the release of most records.
Research over the past decade has shown that opening up notes to patients can improve health care significantly. For example, studies have noted that open records lead to greater medication adherence and help to solve a long-standing issue of patients either feeling confused by their physician’s directions or simply not remembering what was asked of them (DesRoches CM et al, Ann Intern Med 2019;171(1):69–71).
Open notes can improve diagnostic accuracy, diminish stigma, and engage patients in their care. Psychiatric diagnoses have historically suffered from poor inter-rater reliability and could benefit from the patient’s input (Matuszak J and Piasecki M, Psychiatric Times 2012;29(10):12). When patients understand the thinking behind their diagnosis, they are more likely to follow through on treatment and maintain hope in their recovery. Having the patient directly involved in medical decision-making can foster trust, lower demoralization, and increase their sense of control (Thom RP and Farrell HM, AMA J Ethics 2017;19(3):253–259).
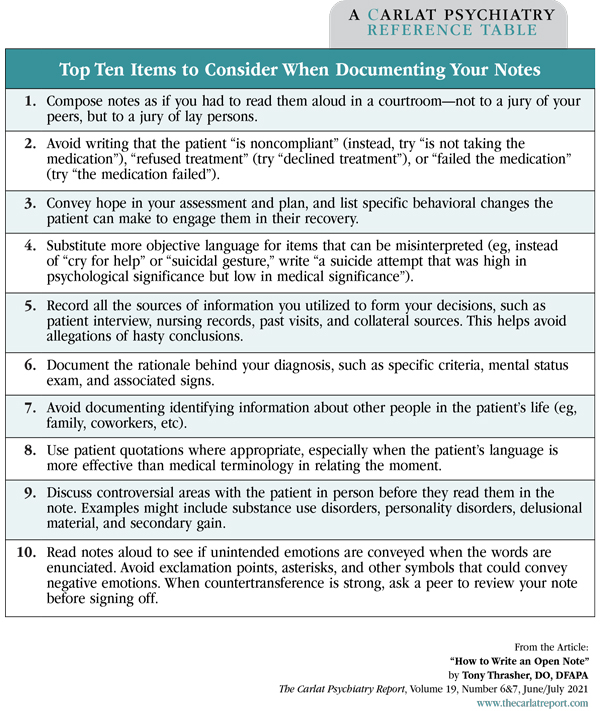
On the other hand, open notes can also lead to miscommunication, complaints, or unspoken resistance between us and those we serve. In the table below, I’ve outlined 10 ways to reduce this risk as you compose your notes in the open era.
Table: Top Ten Items to Consider When Documenting Your Notes
(Click to view full-sized PDF.)
“Either write something worth reading or do something worth writing.” —Benjamin Franklin
TCPR Verdict: New legislation allows patients nearly complete access to their medical record. Open notes are an opportunity to improve patient education, treatment adherence, and the therapeutic relationship. At the very least, write your notes as though your patients will read them.
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2026 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



