The New Billing Codes
Just when you thought you had mastered evaluation and management (E/M) codes, CMS launched a new batch of recommendations for medication management codes (99212–99215). Most changes are for the better. Clinicians can now choose whether to bill based on the time spent on the visit or the complexity of their decision making. The definition of complexity has changed in ways that allow shorter notes and reward clinicians who take care of complex patients.
These changes only affect outpatient visits, although a similar overhaul is in the works for hospitals. The guidelines are challenging to interpret, as they were written with other medical specialties in mind. We’ll translate them here for psychiatric use, and you can read the original text at www.tinyurl.com/d3ucdctu.
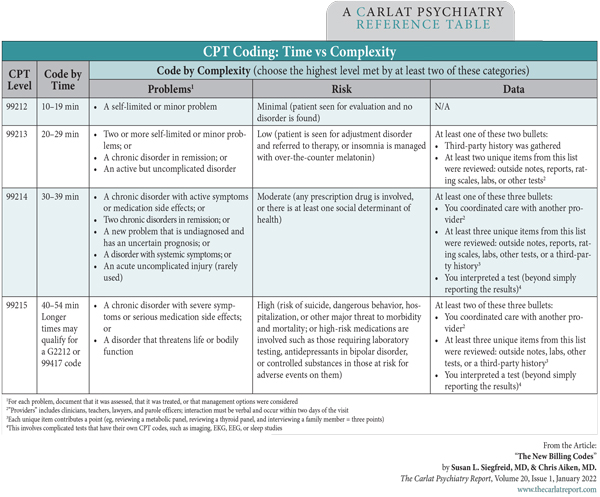
Table: CPT Coding: Time vs Complexity
(Click to view full-size PDF.)
Billing based on time
The new time-based billing is straightforward. Document the total time spent at the visit and select the code based on cutoffs. In addition to face-to-face time, a few other activities count toward time spent as long as they are performed on the visit date. These are:
- Reviewing tests in preparation to see the patient
- Gathering a history from a third party
- Counseling the family or caregivers
- Ordering “medications, tests, or procedures” (eg, labs, cognitive testing) or interpreting those results
- Coordinating care and referring or communicating with other professionals (eg, arranging a psychotherapy referral)
- Writing a progress note
Activities that don’t count include time spent on prior authorizations, traveling to see the patient, and time spent by staff other than yourself.
For established patients, visit times span 10–54 minutes, and longer times (beyond 109 minutes) may be reimbursed with the add-on codes G2212 for Medicare or 99417 for other insurers. Reimbursement for G2212 ranges from $31 in Arkansas and Idaho to $40 in Alaska and Manhattan (Medicare rates are at www.tinyurl.com/2p9uvy4b).
Billing based on complexity
In the old system, “complex” documentation led to lengthy notes that no one had time to read. Now, “complex” means high-risk patients with multiple problems. Instead of turning doctors into scribes, the new guidelines reward physicians who take care of sicker patients, such as hospital discharges, and use treatments that take extra care to manage, such as clozapine, MAOIs, lithium, and ECT.
The new system recognizes what we do more than what we write. Good documentation is still expected, but the specifics of that are left up to the professional. A lengthy review of symptoms no longer counts toward the billable code, but ordering labs, reading old records, interviewing family, and coordinating care with the primary care physician all count.
All this boils down to three categories that determine complexity: problems, risks, and data. Each category is graded from mild (99212) to high (99215), and the final code is based on the highest level in two out of three. The “data” category is difficult to fulfill in mental health, so most of us will rely on the problems and risks.
-
Problems
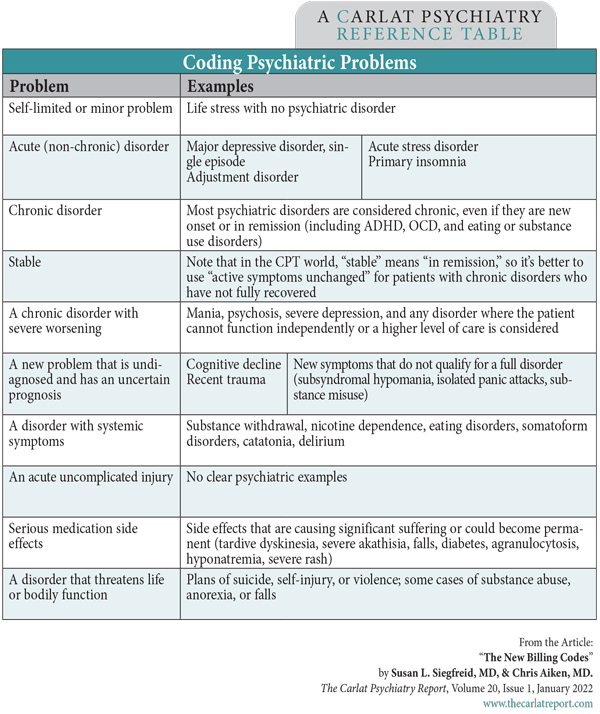
The problem list can include diagnoses, stressors, and nonspecific symptoms like anxiety, bruxism, tremor, and lack of insight. Problems that are severe, high-risk, or chronic count more (most psychiatric disorders are considered chronic). Simply list the problem or use the ICD code (most are in there, including Z63.9 “Problems related to primary support group”), along with your assessment and treatment. See the table below for examples.
Assessment may include history, symptoms, mental status, and rating scales (self-rated scales are allowed). A problem counts if it is “assessed or treated,” meaning problems treated by another clinician may count if they warrant an assessment (eg, metabolic syndrome, sleep apnea, stroke).
Treatment includes any service you provide, from meds to therapy, as well as treatments you recommend but the patient declines. Treatments that are continued count the same as those that are changed, but treatments that involve higher risks may count more in the next category.
-
Risks
The next category is risk, including those posed by the patient’s treatment, diagnosis, and current condition, as well as a new risk factor: social determinants of health. These are factors that get in the way of treatment, including nonadherence, poverty, lack of social support, and inadequate housing or transportation. To document these, write “Diagnosis or treatment significantly limited by social determinants of health, including…” and specify the social problem.
The risk category is relatively easy for psychiatrists to fulfill because prescribing a medication automatically moves the risk level to “moderate.” Outside of that, estimating risk is somewhat arbitrary (for benchmarks, see table CPT Coding: Time vs Complexity above).
-
Data
This category is the most difficult to document, but take heart. By the time you’ve reached a higher CPT level in the data, you are likely treating a complex patient whose problems and risks already fulfill the billing requirements, so documenting the data is icing on the cake. Here’s how to reach the moderate complexity level (99214). Either coordinate care with another provider or review at least three of the following: labs, rating scales, outside records, or a history gathered from the family. Doing both raises the complexity to high (99215), as long as this higher level is also fulfilled by the problems or risks (remember, complexity is determined by the highest score in two out of three categories).
There are other ways to tally the data, but those are the most common permutations in outpatient psychiatry.
Table: Coding Psychiatric Problems
(Click to view full-size PDF.)
Documenting complexity
Use language that matches the coding system. Briefly summarize your assessment (“bipolar II with active hypomania, recent rapid cycling, overall improving”). Specify the risk level and severity, and whether the problem is chronic or not, using the language in our tables.
While simply prescribing medications may raise the complexity level, the spirit of these guidelines is your decision making, and collaborative decision making is valued. To capture this, write “The prescription medication plan is described in the problem list and was developed through shared decision making with the patient, with consideration of the efficacy and safety of the medications and the patient’s preferences in treatment.”
You should still include pertinent aspects of the history, mental status, and review of symptoms in the note, even if they don’t directly influence the CPT code.
New patient visits
E/M codes can also be used for new patients, although most clinicians prefer to bill the 90792 code for this (psychiatric diagnosis with medical services). For new patients, the E/M codes and corresponding time spent are: 99202 (15–29 minutes), 99203 (30–44 minutes), 99204 (45–59 minutes), and (99205 ≥ 60 minutes). Those codes can also be chosen by complexity, in which case the same standards that are used for 99212–99215 apply. Most insurers reimburse 90792 at a higher rate than these 9920- codes, except for 99205, which fetches around 10%–15% more than 90792.
Which to choose? Time vs complexity
Providers who prefer to keep it simple may want to bill by time, but those who treat complex patients will likely be paid more using the complexity system. The choice is yours, and you can flip between the systems as needed. However, when you bill for add-on therapy, the E/M code must be based on complexity (therapy add-on codes are 90833, 16–37 minutes; 90836, 38–52 minutes; and 90838, > 52 minutes).
TCPR Verdict: Whether you bill by time or complexity, the new E/M standards can help you shorten your notes and focus your attention where it needs to be: on the patient.
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2026 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



