Antidepressants: When Dosage Matters
When it comes to dosing antidepressants, it’s often assumed that more is better. While this is true for a few meds, most second-generation antidepressants don’t clearly work better at higher doses. In this article, I’ll review the evidence on antidepressant dose-response relationships and the optimal dose ranges for some antidepressants.
First-generation antidepressantsWhen patients have a poor antidepressant response, clinicians are taught to maximize the antidepressant’s dose before switching medications. Supporting this practice, the American Psychiatric Association (APA) guidelines state that starting doses should be raised slowly, as tolerated, toward a therapeutic dose, and then raised further toward the maximum dose if recovery is not reached (www.tinyurl.com/2r5xuks2). These guidelines are likely evidence-based for first-generation antidepressants, but they are not clearly applicable to the second-generation antidepressants.
Older agents like the monoamine oxidase inhibitors (MAOIs) and tricyclic antidepressants have dose-dependent responses. This means that as the dose is increased, patients usually respond better, within the FDA-approved dose range.
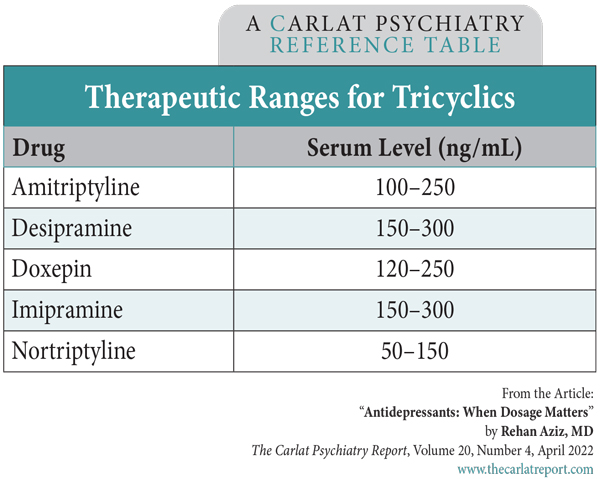
For most psychiatric medications, we can check serum levels to gauge adherence, but with some tricyclics these levels also guide the dosing. Imipramine and amitriptyline show a linear relationship between blood levels and clinical improvement. For nortriptyline, the majority of studies show an inverted “U-shaped” relationship between plasma levels and clinical response. Plasma levels less than 50 ng/mL are inadequate for clinical response, and levels greater than 150 ng/mL are associated with worsening depression. Intermediate levels within a “therapeutic window” of 50–150 ng/mL are necessary for antidepressant response (Amsterdam J et al, Am J Psychiatry 1980;137(6):653–662). The table immediately below lists established therapeutic plasma levels for some tricyclics.Second-generation antidepressantsTable: Therapeutic Ranges for Tricyclics
(Click to view full-size PDF.)
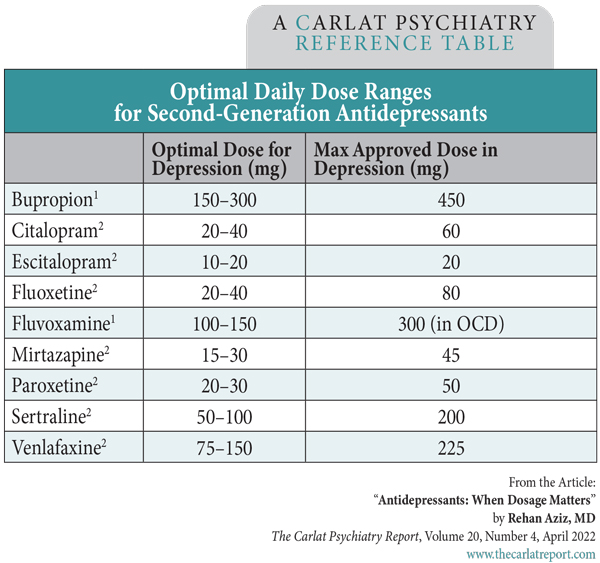
Turning to the second-generation antidepressants, most studies describe a flat dose-response curve, meaning that low doses are just as effective as high doses. A recent meta-analysis by Furukawa and colleagues supports this idea and adds to our understanding of the optimal dose ranges for second-generation drugs (Furukawa TA et al, Lancet Psychiatry 2019;6(7):601–609).
The table at the bottom of the page lists the ideal daily dosage ranges for SSRIs, venlafaxine, and mirtazapine in depression based on Furukawa’s work and other studies.
The takeaway here is to dose and titrate SSRIs, venlafaxine, and mirtazapine to the ranges listed in the table. If your patient doesn’t respond after four to six weeks at the highest optimal dose, then it’s probably time to switch to a new drug. If there’s a partial response, consider adding a second medication.
Table: Optimal Daily Dose Ranges for Second-Generation Antidepressants
(Click to view full-size PDF.)
Awkward conversations
Sometimes, patients insist on raising the dose beyond what the evidence supports, such as increasing sertraline from 50 to 150 mg/day. Many clinicians oblige these requests if they can’t find other agreeable options. If the patient improves, keep in mind that the benefit may be due to the placebo response or the tincture of time. Some patients recover through the natural course of the illness, while others may take longer than four weeks to respond to an antidepressant. Six weeks is recommended for the first antidepressant trial, and a new analysis of the STAR*D trial suggests 12 weeks is necessary to assess the second trial (Rush AJ et al, J Clin Psychiatry 2020;11;81(5):19m12949). A judicious titration downward at a later date, once things have settled down, may be worthwhile.
There’s also the possibility of mood worsening at higher doses. SSRIs can cause some depressing side effects like sleep disruption, low libido, and emotional apathy. In a large randomized controlled trial that compared sertraline at 50, 100, and 200 mg/day in major depression, the higher doses added no benefits but doubled the rate of side effects like agitation, insomnia, sedation, and nausea (Fabre LF et al, Biol Psychiatry 1995;38(9):592–602).
Lastly, patients with comorbidities like anxiety disorders, pain, and OCD may do better with higher doses of SSRIs, as these disorders usually require doses up to the FDA-approved maximum. Also, keep in mind that human variability is wider than these studies can cover. The bell curve suggests that 5% of our patients may fall outside these guidelines, either requiring an unusually high dose or responding to a very low one. For patients who seem to need a very high dose, I’ll try to decrease it when things stabilize to reduce long-term risks.
Carlat Verdict:
Dose SSRIs, venlafaxine, mirtazapine, and bupropion in the low-to-medium ranges to achieve optimal efficacy, while minimizing side effects.
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2026 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



