Deep Rivers Run Quiet. An Update on Social Anxiety Disorder
Steven Hamilton, MD, PhD. The Permanente Medical Group, Department of Psychiatry, Kaiser Permanente San Francisco Medical Center. Dr. Hamilton has no financial relationships with companies related to this material.
Social anxiety disorder (SAD) seems straightforward: an excessive fear of social situations that is treated with cognitive behavioral therapy (CBT) and serotonergic antidepressants. The problem is that many patients don’t respond to these first-line options. In this article, I’ll highlight underutilized treatments that can work when first-line options fail and share tips on how to rule out other causes of this common symptom.
Not normal shyness
Public speaking is one of the most common fears in the US, and almost everyone has experienced a fear of embarrassment. It’s tempting to think that SAD is just an extreme form of these normal fears, but studies suggest otherwise. Over 50% of adults with SAD were not shy earlier in life (Cox BJ et al, Behav Res Ther 2005;43(8):1019–1027). Normal shyness improves with experience, but SAD persists without treatment. These patients avoid major opportunities like dating and work promotions, as well as trivial ones like asking for help in a store.
There are two types of SAD. In the performance subtype, the fear is limited to tasks in public, such as speaking, reading, eating, or using the restroom where one might be observed. Some cases of “test anxiety” and sexual dysfunction are also due to this type of SAD. Isolated performance anxiety responds to beta-blockers, starts later in life, and is less impairing. In the generalized type, the fear expands to multiple situations. Ordering food at a restaurant, making brief comments at a meeting, or approaching someone at a party may all trigger extreme fears of humiliation and judgment.
Underlying both subtypes is a fear of being evaluated and found lacking. Individuals have strict rules about social performance, like believing they must be seen as intelligent, confident, or polite. “If I slip up, they will humiliate me,” “I am not as good as other people,” and “I am weird” are common beliefs. Such patients develop a rigid view of the correct way to act, and therefore lack needed spontaneity and flexibility in their social interactions.
Screening and diagnosis
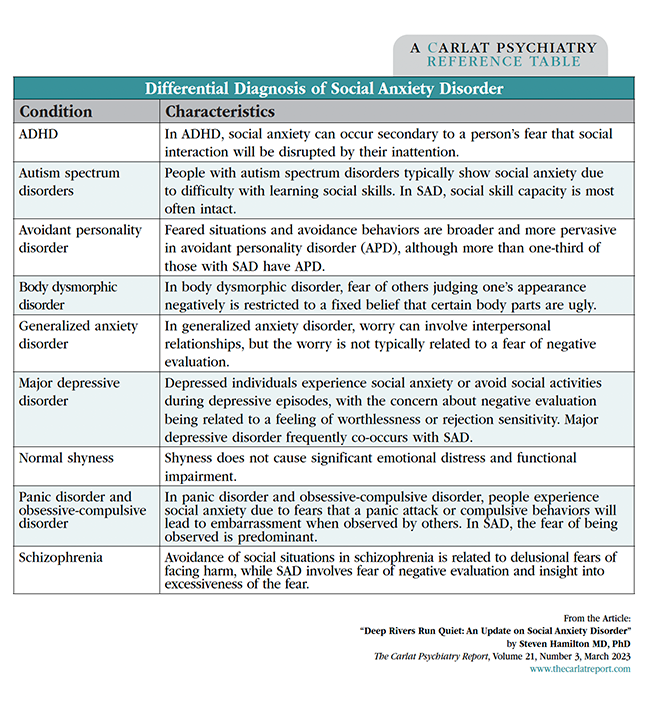
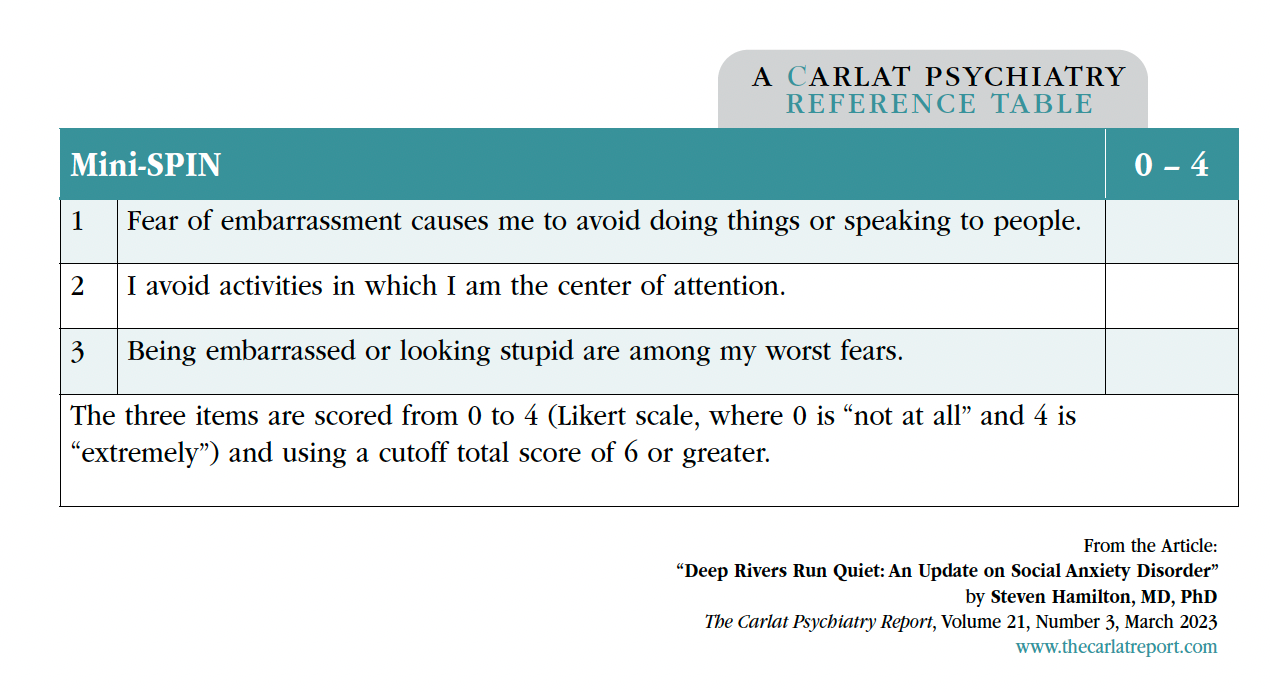
Start with direct questions to screen for SAD, such as those from the Mini-SPIN, a three-question instrument that identifies SAD with a sensitivity and specificity of around 90% (see the “Mini-SPIN” box). Eliciting significant impairments in social and occupational functioning allows straightforward differentiation from normal shyness. The main difficulty is distinguishing these fears from other psychiatric disorders that cause similar symptoms, such as mood disorders, body dysmorphic disorder, autism spectrum disorders, and personality disorders (Leichsenring F and Leweke F, N Engl J Med 2017;376(23):2255–2264; see the table “Differential Diagnosis of Social Anxiety Disorder” for distinguishing features).
Treatments
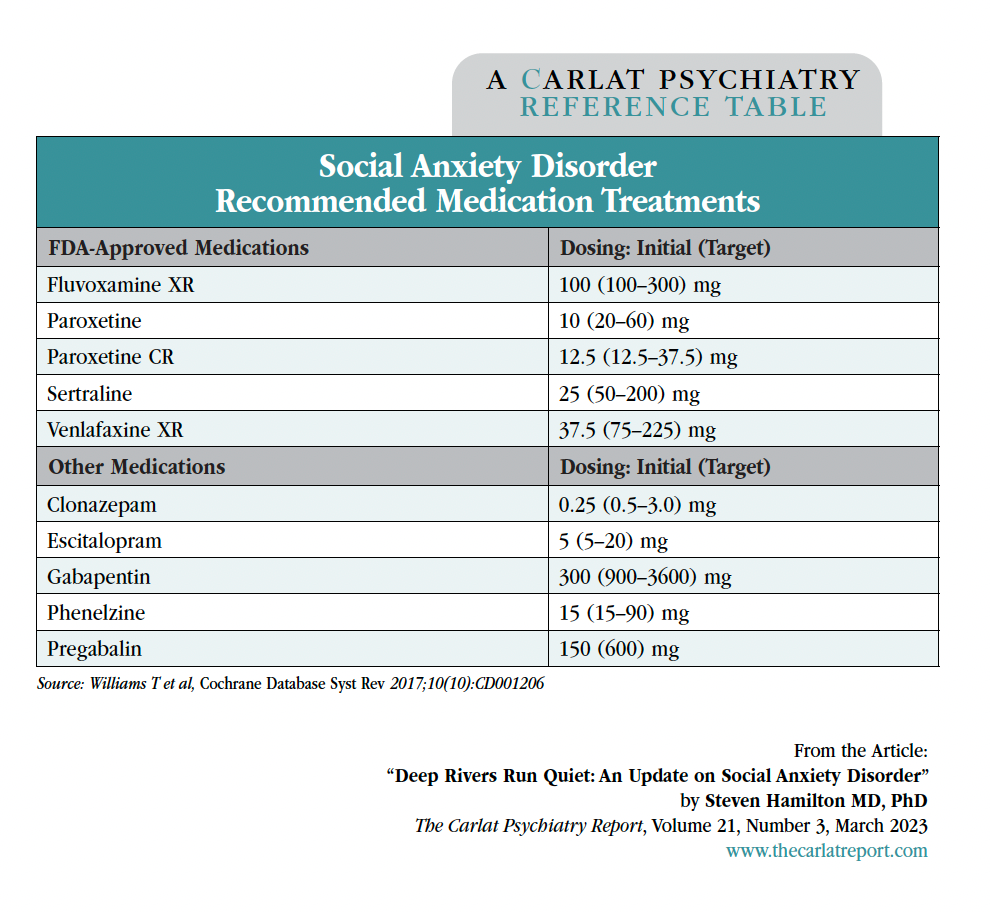
Both psychotherapy and pharmacotherapy are effective for SAD, but CBT is considered first line because it has a more enduring effect, even though medications act a little faster. Among medications, SSRIs and the SNRI venlafaxine are first line for SAD symptoms (Williams T et al, Cochrane Database Syst Rev 2017;10(10):CD001206). There is no evidence that any SSRI is superior to another, but a good first choice is sertraline, which has the best overall tolerability and lowest withdrawal risks among the FDA-approved options. Dosing is similar to that for depression, but the response may be slower. A quarter of patients with no response after two months will have a response after three months (Schneier FR, N Engl J Med 2006;355(10):1029–1036). Start with half of the usual effective target dose for one week and increase after four weeks if there is no response. Treatment should be continued for at least three to six months after clinical response, and usually longer, as relapse is frequent after discontinuation (Blanco C et al, Int J Neuropsychopharmacol 2013;16(1):235–249).
Full recovery is rare with medication, but patients often over-report their progress to please the clinician. To get around this, ask about situations they still avoid—eg, are they comfortable approaching someone at a party, asking questions in class, or asking someone out on a date?
Advanced treatment options
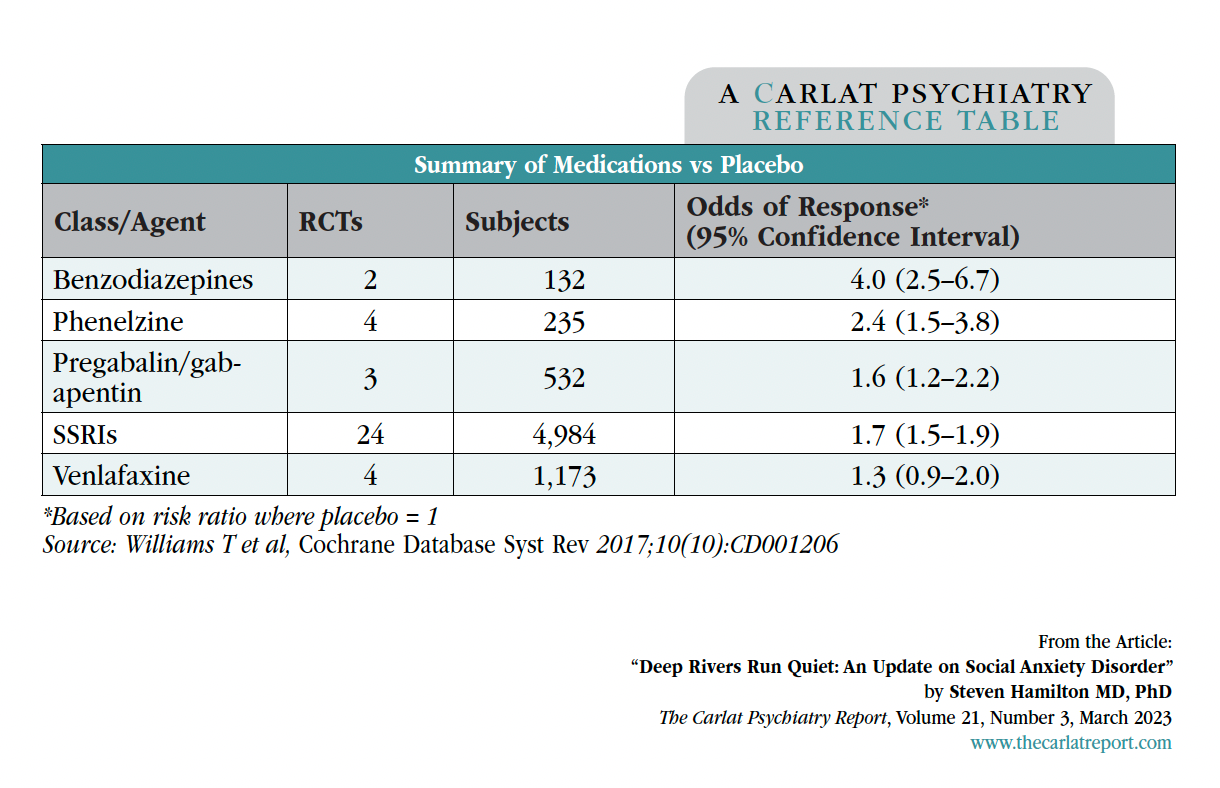
Several medications are worth trying if the patient does not have a meaningful recovery with CBT, SSRIs, and venlafaxine. The MAOI phenelzine is supported by four small randomized controlled trials (RCTs) showing a much stronger effect than SSRIs, with about 60% greater reduction in SAD symptoms (Williams et al, 2017). Pregabalin and gabapentin also have positive RCTs, and can be used as monotherapy or as augmentation for partial response to first-line medications.
Benzodiazepines are effective but best reserved for treatment-resistant cases. Clonazepam has the best evidence (0.5–3.0 mg daily), with studies showing continued benefit at up to one year follow-up. Beyond these options, clinical evidence can tell us what to avoid. Tricyclic antidepressants, bupropion, and atypical antipsychotics have not proven effective in treating SAD, nor have other anticonvulsants or adjunctive buspirone (see the tables “Recommended Medication Treatments” and “Summary of Medications vs Placebo”).
Propranolol and performance anxiety
Beta-blockers are often used for performance anxiety, such as in patients with a fear of public speaking, or in actors and musicians. When 20–40 mg of propranolol is given an hour prior to an anxiety-provoking situation, autonomic symptoms like sweating, tachycardia, and tremor are suppressed. A dozen studies from the 1970s and 1980s showed propranolol was effective for performance anxiety in nonclinical populations, like test-takers, surgeons, dental-phobics, and surgical patients. But there is little clinical trial evidence to support it in clinical populations. In SAD, RCTs of beta-blockers exist only for atenolol, which has not proven effective (Pittelkow MM et al, J Anxiety Disord 2021;78:102357; Williams et al, 2017).
CARLAT VERDICT
SAD is often hidden and requires active inquiry to diagnose. CBT is a first-line treatment, as are SSRIs and venlafaxine. Augmentation with benzodiazepines and pregabalin or gabapentin can be helpful, and phenelzine should always be kept in mind.
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2026 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



