Postpartum Psychosis: A Primer

You receive a call from the OB/GYN service about a 25-year-old woman who delivered a baby girl two days earlier. She seemed to be doing well the day after delivery but is now refusing to see or care for her daughter. She has been unable to sleep and appears confused. You go to her bedside and find her wandering around her room, and you’re unable to engage her in a meaningful interview. From speaking to her husband, you find that she was previously diagnosed with bipolar disorder (BD) in her early 20s but felt stable and stopped mood stabilizers about a year ago.
Postpartum psychosis is a psychiatric emergency that affects one to two out of every 1,000 new mothers (VanderKruik R et al, BMC Psychiatry 2017;17(1):272). Patients with a history of BD are at particularly high risk. Symptoms begin in the first four weeks following childbirth and often develop suddenly, over the course of a single day. Patients display delirium-like symptoms (eg, confusion and waxing and waning of consciousness), manic or depressive symptoms, delusions, hallucinations, disorganized thinking and behavior, and obsessive thoughts regarding the newborn.
Delusions often relate to childbirth and the infant and can include thoughts of altruistic homicide. For example, the mother might believe the only way to save the child from an imaginary danger is to kill them. Or, the delusion might involve a belief that the child has been taken over by an evil entity. Alarmingly, the risk of infanticide during an episode of postpartum psychosis is estimated at about 4% (Brockington I, Arch Womens Ment Health 2017;20(1):63–69). Recognizing and treating postpartum psychosis is crucial to ensure the health and safety of both the parent and the child.
What other diagnoses should you rule out?
 Keep in mind that several diagnoses share features with postpartum psychosis. Substance use can present with similar features, so be sure to obtain urine toxicology tests. Other psychiatric diagnoses to consider include postpartum depression or anxiety disorders, postpartum obsessive-compulsive disorder (OCD), and new-onset schizophrenia. Patients with postpartum depression and anxiety disorders don’t experience delusions or hallucinations, and it’s rare for schizophrenia to have its first onset in the first four weeks postpartum.
Keep in mind that several diagnoses share features with postpartum psychosis. Substance use can present with similar features, so be sure to obtain urine toxicology tests. Other psychiatric diagnoses to consider include postpartum depression or anxiety disorders, postpartum obsessive-compulsive disorder (OCD), and new-onset schizophrenia. Patients with postpartum depression and anxiety disorders don’t experience delusions or hallucinations, and it’s rare for schizophrenia to have its first onset in the first four weeks postpartum.
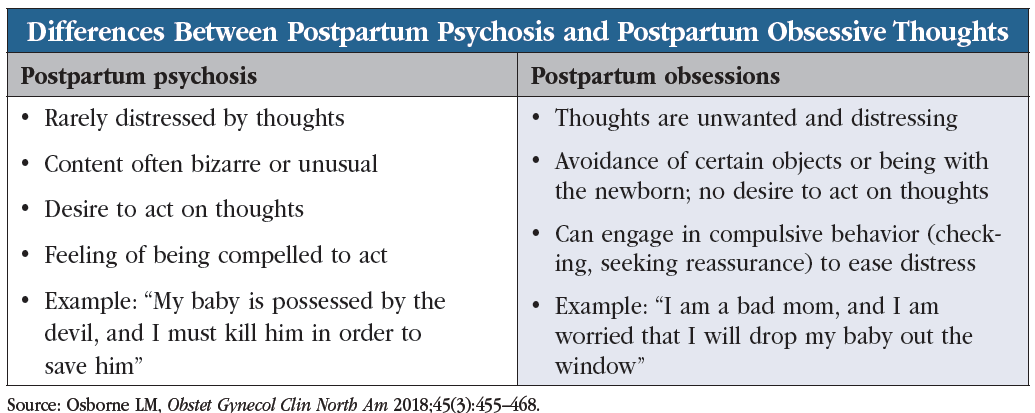
An important diagnosis to rule out is postpartum OCD. The risk of new onset or exacerbation of OCD rises after childbirth, and patients’ intrusive thoughts can be so extreme as to seem delusional. How do you distinguish between postpartum psychosis and the obsessive worrying/intrusive thoughts of postpartum OCD? The obsessive thoughts experienced by new mothers with postpartum OCD are highly distressing, and patients have no intention of acting on them; in contrast, patients with postpartum psychosis often feel compelled to act on those thoughts (see “Differences Between Postpartum Psychosis and Postpartum Obsessive Thoughts” table). Obsessive thoughts are common in patients with postpartum depression, even if they don’t meet full criteria for OCD.
Work closely with the patient’s primary care or OB/GYN provider to rule out medical conditions that can produce acute changes to mental status, including:
- Delirium
- Thyroiditis
- Lupus
- Autoimmune encephalitis
- Medication side effects (eg, steroid-induced mania)
- Sheehan’s syndrome (postpartum pituitary necrosis)
In your evaluation of the patient, she tells you she has no intention to care for or feed her infant daughter because she is convinced the child is dead. She believes the child should be abandoned at the hospital and does not appear distressed by these thoughts.
Risk factors
A history of BD is the strongest risk factor for the development of postpartum psychosis: 20%–30% of postpartum patients with known BD experience postpartum psychosis (Osborne LM, Obstet Gynecol Clin North Am 2018;45(3):455–468). Other risk factors include a prior episode of postpartum psychosis, a family history of BD, sleep loss, and primiparity (ie, a patient’s first childbirth).
Treatment
You transfer the patient to the psychiatric unit and initiate lithium 1200 mg at bedtime and olanzapine 5 mg twice daily, with lorazepam 1 mg as needed for sleep or agitation. Over the next five days she increasingly returns to her baseline and acknowledges she gave birth to a healthy girl. The unit provides a breast pump so she can collect breast milk for the father to take home for the baby.
Postpartum psychosis requires immediate admission to an inpatient facility. Treat postpartum psychosis as you would treat an episode of psychotic mania, ie, with an antipsychotic, a mood stabilizer, and a benzodiazepine for agitation. Compared to other mood stabilizers, lithium appears most effective for postpartum psychosis (Bergink V et al, Am Journ of Psych 2016;173(12):1179–1188). With treatment, most patients (98%) recover within seven weeks (Bergink V et al, Am Journ of Psych 2015;172(2):115–123).
Provide psychoeducation to family members about the importance of sleep, medication adherence, and follow-up appointments with psychiatry and OB/GYN, and inform them that the mother should not be left alone with the child until psychotic symptoms have fully resolved. Once the patient is in remission, you can taper the antipsychotic and the benzodiazepine, but continue lithium as monotherapy for at least nine months. If you see any reason for concern about underlying BD, continue lithium with close monitoring.
If your patient does not respond well to pharmacotherapy after two to four weeks, consider ECT, particularly for patients with psychosis complicated by catatonia, severe agitation, or refusal to eat or drink.
Breastfeeding
Sleep disruption from round-the-clock breastfeeding can prolong the symptoms of postpartum psychosis, so be sure to educate new mothers about the importance of adequate rest. We encourage patients to have their partners or other family members or friends help with nighttime feedings. New mothers can use a breast pump during the day so that the partner can provide a bottle at night, or babies can receive formula.
Is it safe to expose the infant to psychiatric medications through breast milk? Most psychiatric medications pose little risk to breastfeeding infants, although some medications have been studied more than others. Of the antipsychotics, olanzapine and quetiapine have the most data on their safety in breastfeeding (Uguz F, Am J Ther 2021;28(1):118–126). Of the benzodiazepines, lorazepam is preferable to clonazepam, as the latter has been linked with sedation in breastfeeding infants (Soussan C et al, Eur J Clin Pharmacol 2014;70(11):1361–1366).
Infants exposed to lithium through breast milk can develop relatively high blood levels, even higher than those of the mother, especially if the baby is premature (Heinonen E et al, Acta Paediatr 2022;111:1891–1898). Consequently, we are generally hesitant to endorse breastfeeding among women taking lithium. However, some researchers have proposed guidelines for breastfeeding among mothers on lithium, provided that the infants are healthy and full-term and that the mother can ensure frequent checkups for the baby (Imaz ML et al, Front Pharmacol 2021;12:752022). Their recommendations include:
- Engage in a detailed discussion with the mother regarding the risks and benefits of breastfeeding while taking lithium.
- Collaborate with the pediatrician to closely monitor the infant.
- Obtain labs from the baby (lithium level, TSH, BUN, creatinine) at regular intervals, such as at two and 10 days postpartum and then at 30 and 60 days postpartum.
- If the infant’s lithium level is greater than 0.2 mEq/L, or if there are increases in TSH, BUN, or creatinine, recommend that the mother reduce breastfeeding and supplement with formula, or discontinue breastfeeding entirely.
- Educate mothers about potential signs of lithium toxicity in the baby, like lethargy, restlessness, and feeding difficulties.
- Advise mothers to hold off on breastfeeding, or to combine it with formula, during periods when the baby may become dehydrated, such as if the baby has diarrhea or fever.
You can find detailed information about the safety of medications during breastfeeding at the Drugs and Lactation Database (LactMed) (www.tinyurl.com/atnyr6xd).
For a patient with a history of isolated postpartum psychosis who becomes pregnant again, prophylactic treatment can be initiated in late pregnancy or immediately following the subsequent childbirth (see Q&A with Dr. Lauren Osborne in this issue for more on prophylactic treatment for patients with histories of postpartum psychosis).
After nine days on the inpatient unit, the patient is able to return home with her family. You arrange close outpatient follow-up, seeing the patient the day after hospital discharge and weekly thereafter for the following three months. She remains stable and tells you “I realize I need to remain in treatment for my bipolar disorder, not just for my own benefit but now also for my daughter’s.”
CARLAT VERDICT
Postpartum psychosis is a psychiatric emergency affecting about one in 1,000 mothers after childbirth. Individuals with BD are at particularly high risk. Symptoms usually present in the first four weeks after childbirth as delusions, obsessive thoughts, and manic or depressive symptoms. Patients require admission to an inpatient facility and treatment with antipsychotics, benzodiazepines, and lithium. For nursing mothers, select medications with safety data in breastfeeding. Once symptoms resolve, educate patients about the need for prophylactic treatment during future pregnancies.



_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



