Home » How to Talk to Patients About the Risk of Opioid Overdose
How to Talk to Patients About the Risk of Opioid Overdose
February 11, 2020
From The Carlat Addiction Treatment Report
There were 47,600 deaths due to opioid-related overdoses in 2017. Put another way, in the time it’ll take you to read this issue of CATR, almost 5 Americans will die from an opioid overdose (www.cdc.gov/drugoverdose/data/statedeaths.html). One important way to reduce risk is by empowering patients with the knowledge, skills, and tools to prevent and manage overdoses. This article will focus on how to talk to patients to do just that.
Preventing overdose
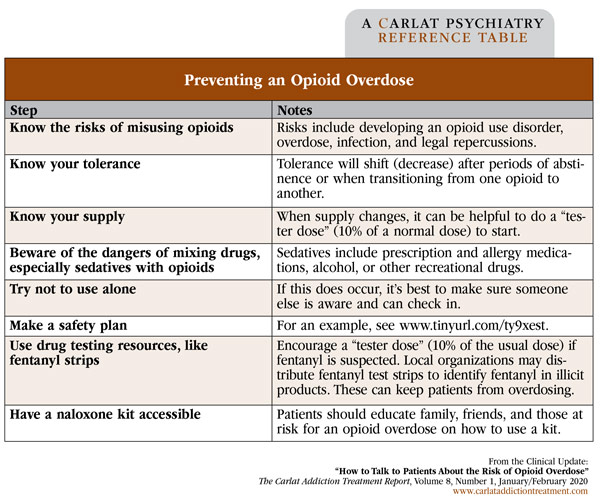
When addressing overdose risk, begin by having your patients tell you about how they use opioids. Your curiosity will help build an alliance with the patient; it’ll also allow you to point out strategies to reduce harm. Be sure to mention specific factors that increase risk, such as concurrent benzodiazepine, gabapentinoid, or alcohol use; the possibility of fentanyl contamination; using alone; and changing dealers. Another high-risk situation is when people come out of incarceration, a hospital, or a residential program. If patients haven’t used any opioids for even a few days and then start taking them again, they’ll be at increased risk of overdose, especially if they go back to their previous amount, because they will have lost their former tolerance (this is called “tolerance shift”). See the table below for discussion points on reducing the risk of overdose. For additional information about how to discuss overdose risk with patients in various settings, see www.prescribetoprevent.org.
Next, talk to your patients about naloxone. In 2018, the US Surgeon General issued a recommendation that more people, including family, friends, and those at risk for opioid overdoses, keep naloxone (Narcan, Evzio) on hand. Ask your patients if they have naloxone at home, if the prescription has been renewed within the last year, if they know how to administer it, and if they’ve instructed others around them on how to use it. Many states have standing orders from medical directors that enable patients and family members to get prescriptions from a pharmacy without seeing a provider.
Assessing for overdose
Be sure to tell your patients to watch for the classic signs of an opioid overdose using language they’ll understand (eg, “cold, clammy hands and bluish lips” instead of “poor perfusion and hypoxia”). If a patient experiences these symptoms, emergent action is required. See “Patient-Centered Guide to Managing an Opioid Overdose” on page 3. (Ed note: A great resource, published by SAMHSA, from which this section was drawn, is the Opioid Overdose Toolkit. It’s available at www.store.samhsa.gov/product/Opioid-Overdose-Prevention-Toolkit/SMA18-4742.)
Good Samaritan laws
Patients engaged in illicit drug use may not want to get involved in a crisis due to fears of legal repercussions, such as arrest, loss of public housing, or loss of benefits. This means many lay responders don’t call 911. As of July 2017, 40 states have passed Good Samaritan laws safeguarding individuals who report an overdose from certain criminal sanctions (Watson DP et al, Harm Reduct J 2018;15(1):18). However, these protections vary by state, and you should know your state’s laws; begin by consulting www.tinyurl.com/wjbojlg.
Good Samaritan laws can include protection from arrest, charge, and prosecution for both controlled substance and paraphernalia possession. For example, New York law protects the individual who is overdosing AND the person who calls 911 from any prosecution for drug possession of alcohol (up to 8 oz; for underage drinkers) or marijuana (any amount), paraphernalia offenses, and sharing of drugs. The law may also provide protection for other crimes, such as probation or parole violations.
These regulations work. Persons with knowledge of Good Samaritan protections or those who have previously used naloxone are more likely to call 911 at the scene of an overdose (Watson, 2018). Furthermore, states with Good Samaritan laws have a lower incidence of opioid-overdose mortality than those without such laws (McClellan C et al, Addict Behav 2018;86:90–95).
CATR Verdict: An important, patient-centered strategy for turning the tide of opioid-related overdose deaths is to talk to your patients about the risks of using opioids and what to do in an emergency. Use language they can understand and encourage patients to train those around them (friends, family, and peers) in the use of lifesaving measures like naloxone.
Addiction TreatmentPreventing overdose
When addressing overdose risk, begin by having your patients tell you about how they use opioids. Your curiosity will help build an alliance with the patient; it’ll also allow you to point out strategies to reduce harm. Be sure to mention specific factors that increase risk, such as concurrent benzodiazepine, gabapentinoid, or alcohol use; the possibility of fentanyl contamination; using alone; and changing dealers. Another high-risk situation is when people come out of incarceration, a hospital, or a residential program. If patients haven’t used any opioids for even a few days and then start taking them again, they’ll be at increased risk of overdose, especially if they go back to their previous amount, because they will have lost their former tolerance (this is called “tolerance shift”). See the table below for discussion points on reducing the risk of overdose. For additional information about how to discuss overdose risk with patients in various settings, see www.prescribetoprevent.org.
Table: Preventing an Opioid Overdose
(Click to view full-size PDF.)
Next, talk to your patients about naloxone. In 2018, the US Surgeon General issued a recommendation that more people, including family, friends, and those at risk for opioid overdoses, keep naloxone (Narcan, Evzio) on hand. Ask your patients if they have naloxone at home, if the prescription has been renewed within the last year, if they know how to administer it, and if they’ve instructed others around them on how to use it. Many states have standing orders from medical directors that enable patients and family members to get prescriptions from a pharmacy without seeing a provider.
Assessing for overdose
Be sure to tell your patients to watch for the classic signs of an opioid overdose using language they’ll understand (eg, “cold, clammy hands and bluish lips” instead of “poor perfusion and hypoxia”). If a patient experiences these symptoms, emergent action is required. See “Patient-Centered Guide to Managing an Opioid Overdose” on page 3. (Ed note: A great resource, published by SAMHSA, from which this section was drawn, is the Opioid Overdose Toolkit. It’s available at www.store.samhsa.gov/product/Opioid-Overdose-Prevention-Toolkit/SMA18-4742.)
Good Samaritan laws
Patients engaged in illicit drug use may not want to get involved in a crisis due to fears of legal repercussions, such as arrest, loss of public housing, or loss of benefits. This means many lay responders don’t call 911. As of July 2017, 40 states have passed Good Samaritan laws safeguarding individuals who report an overdose from certain criminal sanctions (Watson DP et al, Harm Reduct J 2018;15(1):18). However, these protections vary by state, and you should know your state’s laws; begin by consulting www.tinyurl.com/wjbojlg.
Good Samaritan laws can include protection from arrest, charge, and prosecution for both controlled substance and paraphernalia possession. For example, New York law protects the individual who is overdosing AND the person who calls 911 from any prosecution for drug possession of alcohol (up to 8 oz; for underage drinkers) or marijuana (any amount), paraphernalia offenses, and sharing of drugs. The law may also provide protection for other crimes, such as probation or parole violations.
These regulations work. Persons with knowledge of Good Samaritan protections or those who have previously used naloxone are more likely to call 911 at the scene of an overdose (Watson, 2018). Furthermore, states with Good Samaritan laws have a lower incidence of opioid-overdose mortality than those without such laws (McClellan C et al, Addict Behav 2018;86:90–95).
CATR Verdict: An important, patient-centered strategy for turning the tide of opioid-related overdose deaths is to talk to your patients about the risks of using opioids and what to do in an emergency. Use language they can understand and encourage patients to train those around them (friends, family, and peers) in the use of lifesaving measures like naloxone.
Issue Date: February 12, 2020
Table Of Contents
Recommended
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2026 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



