How COVID-19 Affects the Brain
The COVID-19 pandemic is a source of many stress-related conditions, from grief to depression to PTSD. But there’s another problem we need to look out for in those who’ve been infected with the virus: neuropsychiatric effects. The novel coronavirus can potentially invade neurons, and the immune response to this virus can affect the brain as well. Similar viruses like SARS-CoV-1 and MERS-CoV have been implicated in psychiatric disorders, and the first reports of similar problems with COVID-19 are starting to come in (Troyer EA et al, Brain Behav Immun 2020;87:34–39).
Acute neuropsychiatric effects
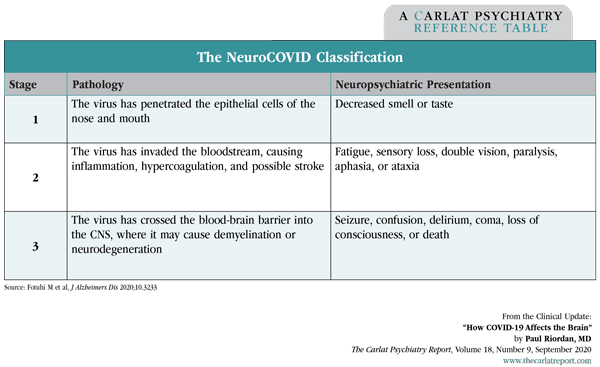
One of the earliest signs of COVID-19 is a neurologic one—decreased sense of smell (anosmia)—which may be due to viral invasion of olfactory epithelial cells. As the illness progresses, more serious neurologic complications can occur, including stroke, seizure, confusion, paralysis, and encephalopathy. One group has proposed a staging system that classifies these symptoms by the degree of viral invasion.
Table: The NeuroCOVID Classification
Neurologic complications are more common in severe than mild COVID-19 cases (6%–15% vs 1%–2%). Among patients who died from COVID-19, 1 in 5 had evidence of encephalopathy. These complications can appear after recovery from the respiratory syndrome and have even been observed in patients with no respiratory symptoms (Rogers JP et al, Lancet Psych 2020;S2215-0366(20)30203-0; Mao L et al, JAMA Neurol 2020;e201127).
You can also expect to see more psychiatric problems after COVID-19 infection. Among the 125 reports of neuropsychiatric complications gathered in a UK database, 1 in 5 had new-onset psychiatric syndromes. Those were: psychosis (43%), dementia-like neurocognitive disorders (26%), and mood disorders (17%) (Varatharaj A et al, Lancet Psych 2020;S2215-0366(20)30287).
Chronic neuropsychiatric effects
If the coronavirus operates like other viruses, patients may remain vulnerable to neuropsychiatric effects long after recovery from the acute illness. It is too early to know the long-term neuropsychiatric effects of COVID-19, but we do have suggestive data from its predecessor, SARS-CoV-1. Rates of psychiatric disorders were markedly elevated 1–2 years after infection with SARS-CoV-1: PTSD (55%), depression (39%), panic disorder (33%), and OCD (16%). Prior to infection, the rate of any psychiatric diagnosis was just 3%—probably an underestimation due to cultural stigma and financial incentives to underreport when applying for the SARS survivors’ fund (Lam M et al, Arch Int Med 2009;169(22):2142–2147). Those numbers are alarming, but they don’t tell us whether the disorders were due to direct effects of the virus or the various stressors surrounding it.
Chronic cognitive problems are also possible. Most viruses that infect the CNS cause lasting cognitive problems, including HIV, HSV (herpes), and SARS. Nearly 1 in 5 persons with SARS reported problems with concentration or memory weeks to months post-illness, and many of them were under age 40 (Rogers JP et al, Lancet Psych 2020).
Viral illnesses can also affect future generations. For example, the offspring of mothers exposed to the 1957 influenza type A2 virus had an elevated risk of schizophrenia (Mednick SA et al, Arch Gen Psych 1988;45(2):189–192).
Treatment
Until we know more about its neuropsychiatric effects, it’s best to treat the syndromes that present after COVID-19 infection as you would any other case, with a few modifications:
- Pay attention to cognitive symptoms like memory, attention, and processing speed. If these persist longer than 6 months after infection, consider referral to a neurologist.
- Aerobic exercise (eg, 30 minutes a day of any activity that raises the heart rate by 10 bpm) and a heart-healthy diet (see TCPR, May 2019) are currently recommended as first-line interventions for cognitive problems after COVID-19.
- Those with significant cognitive impairments may benefit from cognitive rehabilitation with a therapist who works with stroke, head injury, or dementia.
- Consider testing for inflammation when post-COVID-19 depression does not respond to treatment. This can be measured with a test—the high-sensitivity C-reactive protein (CRP)—where levels above 3 indicate inflammation. Depressions that arise out of inflammatory states respond better to dopaminergics, bupropion, or tricyclics than to SSRIs (see TCPR, Feb 2020).
- Normalizing that a psychiatric illness may be due to COVID-19 infection might comfort some patients who struggle with the stigma of a psychiatric diagnosis.
TCPR Verdict: Psychiatric problems are likely to persist long after the COVID-19 pandemic resolves, whether from the stress of the illness or from the virus’s direct effects on the brain.
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2026 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



