Home » Suicide Safety Planning for the Patient with Addiction
Suicide Safety Planning for the Patient with Addiction
November 5, 2021
From The Carlat Addiction Treatment Report
Jessica Casella, LCSW
Private practice social worker, Branford, CT. Adjunct faculty member at Sacred Heart University School of Social Work. Active member of the state of Connecticut’s Suicide Advisory Board.
Ms. Casella has disclosed no relevant financial or other interests in any commercial companies pertaining to this educational activity.
Suicide is an epidemic in itself, with over 45,000 completed suicides in 2019 alone. It is the 10th leading cause of death in the US and the second among people ages 10–34 (Cerel J et al, Suicide Life Threat Behav 2019;49(2):529–534). With media attention focused on the growing number of accidental overdose deaths, suicide among people with addiction may not always be at the forefront of clinicians’ minds; however, people with addiction are at a much higher risk of suicide than the general population.
Suicide and addiction
Substances are frequently involved in suicide attempts. Alcohol and opioids are each implicated in a fifth of suicides, followed by cannabis (10.2%), cocaine (4.6%), and amphetamines (3.4%) (Esang M and Ahmed S, Am J Psych Residents 2018;13(6):6–8). A tobacco use disorder diagnosis is associated with double the suicide risk, and a person with tobacco, drug, and alcohol use disorders has more than an 11-fold increased risk of suicide (Lynch FL et al, Addict Sci Clin Pract 2020;15(1):14).
Unfortunately, we don’t have a reliable way of knowing who might attempt suicide or when they might make the attempt. The best tool available for clinicians is a thorough suicide risk assessment, and the Substance Abuse and Mental Health Services Administration (SAMHSA) recommends conducting one during all initial appointments for patients with addiction (www.tinyurl.com/wte6sn4c).
Many clinicians prefer standardized risk assessment tools. We recommend the Columbia-Suicide Severity Rating Scale (C-SSRS), the Suicide Assessment Five-Step Evaluation and Triage (SAFE-T) Tool, or the Ask Suicide Screening Questions (ASQ) Toolkit.
In addition to the risk assessment, any patient categorized as high risk for suicide should engage in safety planning before walking out of your office.
What is safety planning?
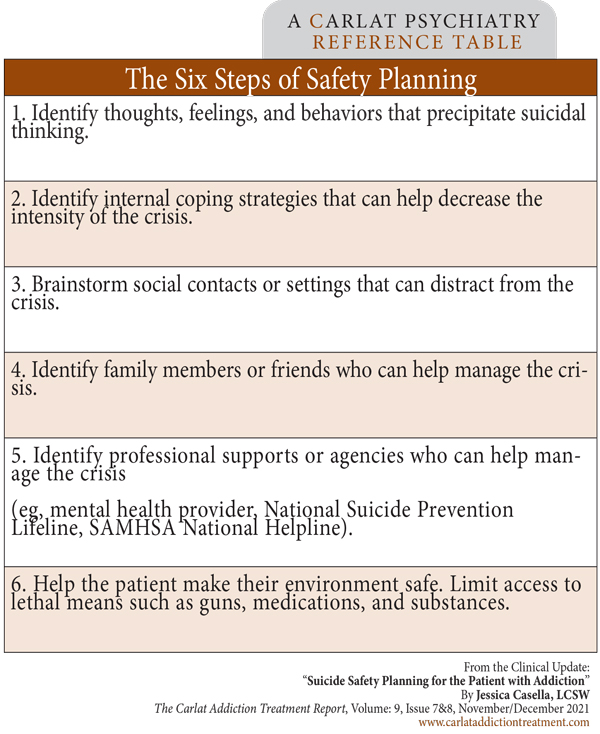
Safety planning is a six-step process in which clinicians and patients work together to write a safety plan—a document that patients can use to prevent a suicidal crisis (Stanley B and Brown G, Cog Beh Practice 2012;19(2):256–264). Research has shown that safety planning can decrease suicidal behavior, increase treatment engagement, and minimize days in the hospital (Stanley B et al, JAMA Psychiatry 2018;75(9):894–900; Bryan CJ et al, J Affect Disord 2017;212:64–72). It’s usually done on paper, but can be done electronically as well—see www.tinyurl.com/4pdcts6c for an example of an app, and search online for resources on social media platforms and in other languages. At the end of a safety planning session, the patient should have a straightforward and easy-to-read list of steps that will help keep them safe. Here are the steps (also see the box below).
Step 1: Identifying the crisis
This first step helps patients identify when suicidal thinking might be on the way. Issues like loneliness, relationship difficulties, financial strain, mental illness, and of course addiction are all potential catalysts of suicidal thinking. Helping patients recognize triggers for substance use will in turn help them recognize circumstances that could lead to suicidal thinking or a suicide attempt.
Step 2: Coping
Here patients come up with ways to distract themselves from suicidal thoughts when they occur. Common coping strategies include exercising, listening to music, and watching movies. Many patients with addiction are used to turning to substances to feel better, so be explicit about what constitutes healthy and unhealthy coping strategies. The more specific the strategy, the better it is; for example, a patient should write “Watch Caddyshack” instead of “Watch something funny.”
One excellent strategy is making a “hope box”—a group of tangible reminders of why it is worth staying alive. Have patients gather photos, quotes, sobriety chips/coins, or anything personally meaningful, and have them store these items together so they can be reviewed when the patient is feeling suicidal (Stanley B et al, J Am Acad Child Adolesc Psych 2009;48(10):1005–1013). Virtual Hope Box is an app that patients can use to create a digital hope box (www.tinyurl.com/wuwk9rxf).
Steps 3–5: Listing of supports in three categories
Patients should have a list of people to reach out to in a time of suicidal crisis. The midst of this crisis is not the time to look up phone numbers, so make sure contact information is part of the plan. A safety plan should have three contact lists on it: social contacts, friends/family, and professionals. Many patients with addiction have friends in recovery or sponsors that can serve as supports in a time of crisis. Peer groups like Alcoholics Anonymous (AA) can be great sources of support as well.
Step 6: Lethal means safety counseling
Lethal means safety counseling is all about creating a safe environment. Amazingly, in a quarter of cases, less than five minutes separate the decision to attempt suicide and the attempt itself (Simon OR et al, Suicide Life Threat Behav 2001;32(1 Suppl):49–59). Delaying access to lethal means by just a few minutes can literally be life-saving. Family and friends are especially helpful when creating a safe living environment, so involve them early if possible.
Lethal means safety counseling starts with identifying the means of suicide your patient has access to—guns and medication are the most common—and seeing which of these can be removed from the patient’s living environment. For example, store guns outside of the house, sell them, or dispose of them through gun buyback events. Dispose of excess medication safely at a police station or DEA dropoff site (www.tinyurl.com/brbc7smk). Medication destruction kits are available online.
If a patient won’t give up their gun, encourage gun locks, safes, and separate ammunition storage. If a necessary medication carries overdose potential, store it in a lockbox or blister pack, or have it prescribed in smaller quantities. Seemingly small steps can have huge effects. For example, suicide deaths by acetaminophen overdose dropped 43% in the UK after the government required pills to be sold in small blister packs (Hawkton K et al, BMJ 2013;346:f403). The key is to make sure patients can’t easily get their hands on lethal means at an impulsive moment.
For patients with addiction, lethal means safety counseling also involves limiting access to substances. The conversations to have are similar to ones you probably have with patients all the time: Counsel them to get rid of drugs and alcohol in the house, delete dealer contact information, and consider switching numbers so dealers can’t get in touch. Medications for opioid use disorders decrease mortality, but be particularly aware if these medications are suddenly stopped as this is a particularly high-risk period (Bohnert ASB and Ilgen MA, N Engl J Med 2019;380(1):71–79).
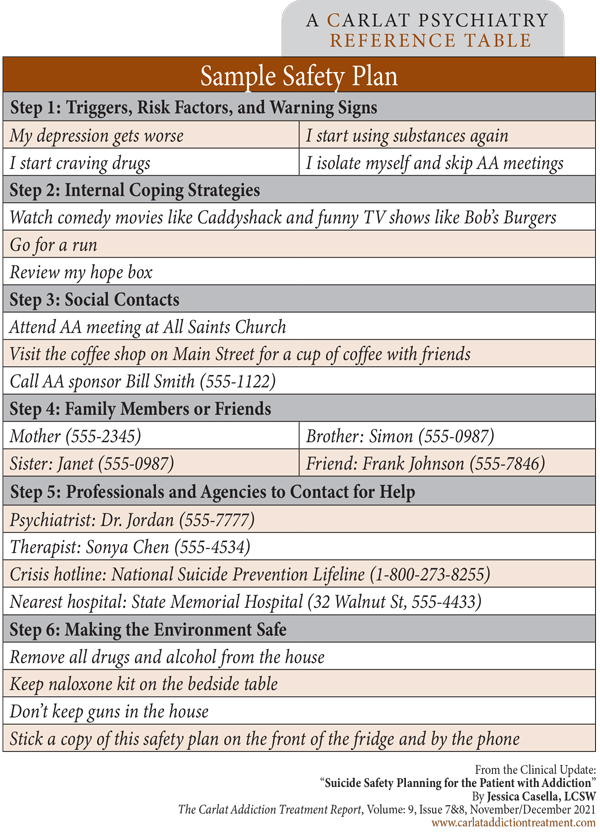
See the adjacent table for a sample of a completed safety plan. For more detailed information about the steps of safety planning, see: www.tinyurl.com/2dd55uwxz
Wrapping up
At the end of a safety planning session, patients should walk out of your office (or the emergency room) holding a physical, easy-to-read document. Have them put a copy on the fridge, in the car, on their bedside table, or anywhere it will be visible and easy to find. Remind patients that the plan won’t help them if they can’t find it when they need it.
Finally, remember to review your patients’ safety plans regularly. Many clinicians find it helpful to review plans at set intervals, such as every six months. Transitions in care are particularly vulnerable times, so always make sure to review the safety plan when patients change providers or level of care.
CATR Verdict: Addiction is a major risk factor for suicide, so perform a suicide risk assessment on all patients with a substance use disorder and engage in the six steps of safety planning with anyone who is high risk. Be sure that patients have a physical copy of their safety plan and that they keep it accessible. Review the plan at set intervals, at least every six months.
Addiction TreatmentSuicide and addiction
Substances are frequently involved in suicide attempts. Alcohol and opioids are each implicated in a fifth of suicides, followed by cannabis (10.2%), cocaine (4.6%), and amphetamines (3.4%) (Esang M and Ahmed S, Am J Psych Residents 2018;13(6):6–8). A tobacco use disorder diagnosis is associated with double the suicide risk, and a person with tobacco, drug, and alcohol use disorders has more than an 11-fold increased risk of suicide (Lynch FL et al, Addict Sci Clin Pract 2020;15(1):14).
Unfortunately, we don’t have a reliable way of knowing who might attempt suicide or when they might make the attempt. The best tool available for clinicians is a thorough suicide risk assessment, and the Substance Abuse and Mental Health Services Administration (SAMHSA) recommends conducting one during all initial appointments for patients with addiction (www.tinyurl.com/wte6sn4c).
Many clinicians prefer standardized risk assessment tools. We recommend the Columbia-Suicide Severity Rating Scale (C-SSRS), the Suicide Assessment Five-Step Evaluation and Triage (SAFE-T) Tool, or the Ask Suicide Screening Questions (ASQ) Toolkit.
In addition to the risk assessment, any patient categorized as high risk for suicide should engage in safety planning before walking out of your office.
What is safety planning?
Safety planning is a six-step process in which clinicians and patients work together to write a safety plan—a document that patients can use to prevent a suicidal crisis (Stanley B and Brown G, Cog Beh Practice 2012;19(2):256–264). Research has shown that safety planning can decrease suicidal behavior, increase treatment engagement, and minimize days in the hospital (Stanley B et al, JAMA Psychiatry 2018;75(9):894–900; Bryan CJ et al, J Affect Disord 2017;212:64–72). It’s usually done on paper, but can be done electronically as well—see www.tinyurl.com/4pdcts6c for an example of an app, and search online for resources on social media platforms and in other languages. At the end of a safety planning session, the patient should have a straightforward and easy-to-read list of steps that will help keep them safe. Here are the steps (also see the box below).
Step 1: Identifying the crisis
This first step helps patients identify when suicidal thinking might be on the way. Issues like loneliness, relationship difficulties, financial strain, mental illness, and of course addiction are all potential catalysts of suicidal thinking. Helping patients recognize triggers for substance use will in turn help them recognize circumstances that could lead to suicidal thinking or a suicide attempt.
Step 2: Coping
Here patients come up with ways to distract themselves from suicidal thoughts when they occur. Common coping strategies include exercising, listening to music, and watching movies. Many patients with addiction are used to turning to substances to feel better, so be explicit about what constitutes healthy and unhealthy coping strategies. The more specific the strategy, the better it is; for example, a patient should write “Watch Caddyshack” instead of “Watch something funny.”
One excellent strategy is making a “hope box”—a group of tangible reminders of why it is worth staying alive. Have patients gather photos, quotes, sobriety chips/coins, or anything personally meaningful, and have them store these items together so they can be reviewed when the patient is feeling suicidal (Stanley B et al, J Am Acad Child Adolesc Psych 2009;48(10):1005–1013). Virtual Hope Box is an app that patients can use to create a digital hope box (www.tinyurl.com/wuwk9rxf).
Steps 3–5: Listing of supports in three categories
Patients should have a list of people to reach out to in a time of suicidal crisis. The midst of this crisis is not the time to look up phone numbers, so make sure contact information is part of the plan. A safety plan should have three contact lists on it: social contacts, friends/family, and professionals. Many patients with addiction have friends in recovery or sponsors that can serve as supports in a time of crisis. Peer groups like Alcoholics Anonymous (AA) can be great sources of support as well.
Step 6: Lethal means safety counseling
Lethal means safety counseling is all about creating a safe environment. Amazingly, in a quarter of cases, less than five minutes separate the decision to attempt suicide and the attempt itself (Simon OR et al, Suicide Life Threat Behav 2001;32(1 Suppl):49–59). Delaying access to lethal means by just a few minutes can literally be life-saving. Family and friends are especially helpful when creating a safe living environment, so involve them early if possible.
Lethal means safety counseling starts with identifying the means of suicide your patient has access to—guns and medication are the most common—and seeing which of these can be removed from the patient’s living environment. For example, store guns outside of the house, sell them, or dispose of them through gun buyback events. Dispose of excess medication safely at a police station or DEA dropoff site (www.tinyurl.com/brbc7smk). Medication destruction kits are available online.
If a patient won’t give up their gun, encourage gun locks, safes, and separate ammunition storage. If a necessary medication carries overdose potential, store it in a lockbox or blister pack, or have it prescribed in smaller quantities. Seemingly small steps can have huge effects. For example, suicide deaths by acetaminophen overdose dropped 43% in the UK after the government required pills to be sold in small blister packs (Hawkton K et al, BMJ 2013;346:f403). The key is to make sure patients can’t easily get their hands on lethal means at an impulsive moment.
For patients with addiction, lethal means safety counseling also involves limiting access to substances. The conversations to have are similar to ones you probably have with patients all the time: Counsel them to get rid of drugs and alcohol in the house, delete dealer contact information, and consider switching numbers so dealers can’t get in touch. Medications for opioid use disorders decrease mortality, but be particularly aware if these medications are suddenly stopped as this is a particularly high-risk period (Bohnert ASB and Ilgen MA, N Engl J Med 2019;380(1):71–79).
See the adjacent table for a sample of a completed safety plan. For more detailed information about the steps of safety planning, see: www.tinyurl.com/2dd55uwxz
Table: The Six Steps of Safety Planning
(Click to view full-sized PDF.)
Wrapping up
At the end of a safety planning session, patients should walk out of your office (or the emergency room) holding a physical, easy-to-read document. Have them put a copy on the fridge, in the car, on their bedside table, or anywhere it will be visible and easy to find. Remind patients that the plan won’t help them if they can’t find it when they need it.
Finally, remember to review your patients’ safety plans regularly. Many clinicians find it helpful to review plans at set intervals, such as every six months. Transitions in care are particularly vulnerable times, so always make sure to review the safety plan when patients change providers or level of care.
CATR Verdict: Addiction is a major risk factor for suicide, so perform a suicide risk assessment on all patients with a substance use disorder and engage in the six steps of safety planning with anyone who is high risk. Be sure that patients have a physical copy of their safety plan and that they keep it accessible. Review the plan at set intervals, at least every six months.
Table: Sample Safety Plan
(Click to view full-sized PDF.)
Issue Date: November 5, 2021
Table Of Contents
Recommended
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2026 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



