Home » Buprenorphine Induction Without Withdrawal
Buprenorphine Induction Without Withdrawal
November 5, 2021
From The Carlat Addiction Treatment Report
David Moltz, MD.
Dr. Moltz has disclosed no relevant financial or other interests in any commercial companies pertaining to this educational activity.
REVIEW OF: Ahmed S et al, Am J Addict 2021;30(4):305–315
Buprenorphine is notorious for precipitating withdrawal in patients who have recently taken opioids. Its high receptor affinity and partial agonism at the mu receptor can make inductions tricky. Giving it too soon can cause severe withdrawal, yet giving it too late means patients are in discomfort from withdrawal while awaiting their first buprenorphine dose. A fair number of inductions result in some level of precipitated withdrawal (estimates range from 5% to 16.8%), and it has been speculated that the higher prevalence of fentanyl on the street has increased this rate even further. But there may be an alternative.
This review examined a novel approach, called microinduction, for transitioning patients to buprenorphine from an opioid agonist like methadone or heroin. In this strategy, microdoses of buprenorphine (0.2–0.5 mg) are introduced and gradually increased without waiting for withdrawal to start. Microinduction is based on the theory that multiple small doses of buprenorphine, given its high receptor affinity, will gradually replace the lower-affinity opioid that is occupying the mu receptor sites. This gradual change from full to partial agonist causes a less dramatic physiological shift, and hence fewer withdrawal symptoms. In contrast, a single large dose of buprenorphine will quickly replace the opioid and result in a sudden drop in agonist signaling.
This literature review examined 18 reports (n = 63) of various buprenorphine microinduction strategies. The individual studies were quite heterogeneous, varying in opioid agonists, buprenorphine dosing, and time course. However, they all started with very low doses of buprenorphine (0.2–0.5 mg) and increased this dose slowly over time (3–112 days). Most transitioned over 4–8 days and stabilized patients on daily buprenorphine doses of 8–16 mg. Some utilized symptomatic treatment with clonidine during the induction period.
In most cases, the opioid agonist was continued while buprenorphine was introduced, then tapered over time or discontinued when the buprenorphine dose was judged adequate. Six studies chose instead to utilize a transdermal patch, given its ability to consistently deliver small amounts of medication. These patches (buprenorphine in all cases, save one that used fentanyl) served as a bridge from full agonist to eventual higher doses of sublingual buprenorphine. In most but not all of these cases, the previous opioid was discontinued when the transdermal patch was started.
The review highlights a few situations in which microinduction might be particularly beneficial, namely when transitioning to buprenorphine from methadone and for patients with chronic pain. The long half-life of methadone makes for an extended withdrawal period when utilizing traditional buprenorphine induction. Patients in this study were transitioned from methadone doses as high as 200 mg without requiring prior decrease of dose. Patients hospitalized for medical or surgical conditions could transition from illicit opioids without withdrawal. Individuals with chronic pain were transitioned without having to endure an increase in pain during the opioid withdrawal period.
Before we jump to microinduction for all of our patients, there are caveats to consider. All of these papers were case reports or case series, with only one open-label trial. Most did not evaluate withdrawal with validated measures. There is no standard protocol for microinduction and no randomized trials comparing microinduction to the usual method of induction. Nevertheless, this review shows the promise of this technique as an alternative for safe, effective initiation of buprenorphine treatment.
CATR’s Take
While not yet standard of care, microinduction could be considered for patients who are difficult to induce. However, there is still work to do in standardizing and validating this approach.
Addiction TreatmentBuprenorphine is notorious for precipitating withdrawal in patients who have recently taken opioids. Its high receptor affinity and partial agonism at the mu receptor can make inductions tricky. Giving it too soon can cause severe withdrawal, yet giving it too late means patients are in discomfort from withdrawal while awaiting their first buprenorphine dose. A fair number of inductions result in some level of precipitated withdrawal (estimates range from 5% to 16.8%), and it has been speculated that the higher prevalence of fentanyl on the street has increased this rate even further. But there may be an alternative.
This review examined a novel approach, called microinduction, for transitioning patients to buprenorphine from an opioid agonist like methadone or heroin. In this strategy, microdoses of buprenorphine (0.2–0.5 mg) are introduced and gradually increased without waiting for withdrawal to start. Microinduction is based on the theory that multiple small doses of buprenorphine, given its high receptor affinity, will gradually replace the lower-affinity opioid that is occupying the mu receptor sites. This gradual change from full to partial agonist causes a less dramatic physiological shift, and hence fewer withdrawal symptoms. In contrast, a single large dose of buprenorphine will quickly replace the opioid and result in a sudden drop in agonist signaling.
This literature review examined 18 reports (n = 63) of various buprenorphine microinduction strategies. The individual studies were quite heterogeneous, varying in opioid agonists, buprenorphine dosing, and time course. However, they all started with very low doses of buprenorphine (0.2–0.5 mg) and increased this dose slowly over time (3–112 days). Most transitioned over 4–8 days and stabilized patients on daily buprenorphine doses of 8–16 mg. Some utilized symptomatic treatment with clonidine during the induction period.
In most cases, the opioid agonist was continued while buprenorphine was introduced, then tapered over time or discontinued when the buprenorphine dose was judged adequate. Six studies chose instead to utilize a transdermal patch, given its ability to consistently deliver small amounts of medication. These patches (buprenorphine in all cases, save one that used fentanyl) served as a bridge from full agonist to eventual higher doses of sublingual buprenorphine. In most but not all of these cases, the previous opioid was discontinued when the transdermal patch was started.
The review highlights a few situations in which microinduction might be particularly beneficial, namely when transitioning to buprenorphine from methadone and for patients with chronic pain. The long half-life of methadone makes for an extended withdrawal period when utilizing traditional buprenorphine induction. Patients in this study were transitioned from methadone doses as high as 200 mg without requiring prior decrease of dose. Patients hospitalized for medical or surgical conditions could transition from illicit opioids without withdrawal. Individuals with chronic pain were transitioned without having to endure an increase in pain during the opioid withdrawal period.
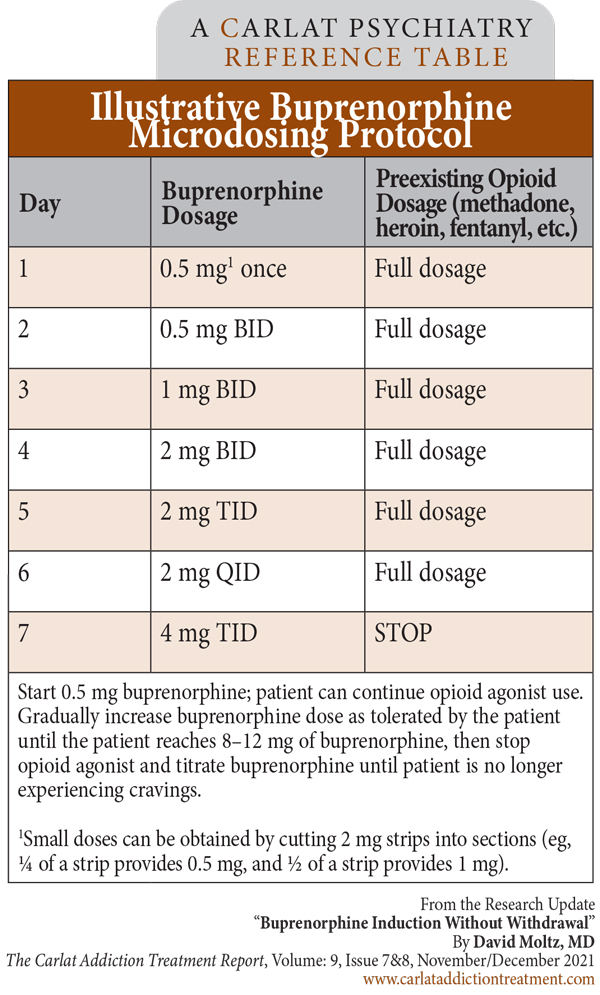
Table: Illustrative Buprenorphine Microdosing Protocol
(Click to view full-sized PDF.)
Before we jump to microinduction for all of our patients, there are caveats to consider. All of these papers were case reports or case series, with only one open-label trial. Most did not evaluate withdrawal with validated measures. There is no standard protocol for microinduction and no randomized trials comparing microinduction to the usual method of induction. Nevertheless, this review shows the promise of this technique as an alternative for safe, effective initiation of buprenorphine treatment.
CATR’s Take
While not yet standard of care, microinduction could be considered for patients who are difficult to induce. However, there is still work to do in standardizing and validating this approach.
KEYWORDS buprenorphine buprenorphine-induction medication-of-opioid-use-disorder-moud opioid-use-disorder
Issue Date: November 5, 2021
Table Of Contents
Recommended
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2026 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



