Home » Responding to Sexual Activity on the Inpatient Psychiatric Unit
Responding to Sexual Activity on the Inpatient Psychiatric Unit
March 23, 2022
From The Carlat Hospital Psychiatry Report
Husna Najand, MD.
Olive View—UCLA Psychiatry Residency Program.
Dr. Najand has disclosed no relevant financial or other interests in any commercial companies pertaining to this educational activity.
We know sexual attraction occurs among individuals staying together in a psychiatric inpatient unit. The prevalence of sexual activity on acute units is as high as 5%—and up to 70% among chronically ill patients in long-term residence in state hospitals (Ford E et al, Psychiatr Serv 2003;54(3):346–350; Wright ER et al, Journal of Ethics in Mental Health 2012;7:1–5). However, there are no universal policies addressing sexual activity between patients on inpatient units, and Joint Commission standards do not include any discussion of this topic.
Hospital policies regarding physical contact
Many psychiatric hospitals lack specific policies on patient-to-patient physical contact. Perhaps these policies are absent because hospital administrators view such contact as obviously inappropriate, for a variety of reasons. Sexual contact elicits strong emotions, both positive and negative, that may distract from or interfere with treatment. If sexual contact is non-consensual or involves patients with reduced capacity, it can be both criminal and psychologically damaging.
What about more casual physical contact, such as holding hands, sitting very close to others, or hugging? Patients often make intense connections with others in inpatient units, given the encouragement to be honest and self-revealing in treatment groups. Touching may seem like a natural extension of emotional intimacy. Nonetheless, there is a slippery slope from friendly touching to sex, so most units err on the side of caution and completely prohibit physical contact between patients. Generally, we agree that such policies are prudent. We remind patients of these policies at the beginning of and during the course of their inpatient stays, particularly when they display hypersexual behaviors.
How to respond to sexual contact in the hospital
The nursing or security staff inform you that two patients on the unit have engaged in sexual activity. What do you do next? First, determine what type of sexual activity occurred. In most cases on inpatient units, sexual activity occurs between fully clothed individuals and involves kissing, hugging, and fondling. Actual sexual intercourse is rare. You will generally have a good idea of what happened from the reports of the unit staff who discovered the activity, but you should do your best to confirm this when you interview the patients yourself. Separate the patients and place them under 1:1 supervision while you evaluate each privately. Patients should not change clothing or take showers during this time, as physical evidence may be needed. Be sure to inform the hospital’s risk management office of the incident.
Determine capacity to consent
Regardless of the nature of the activity, you should try to determine whether the patients had the capacity to consent to sexual activity. All individuals—including those with severe mental illness, as well as those with intellectual disabilities or dementia—have sexual consent capacity once they reach the age of consent as established by their state. Patients on psychiatric holds also retain sexual consent capacity; the exception is if a court previously determined a patient lacks capacity, such as in probate conservatorship. Assuming the patients involved are their own decision makers, how do you determine if they really have the capacity to consent to sexual activity? While each state has its own statutes, the following principles have typically been used to determine sexual consent capacity (Boni-Saenz AA, Psychiatric Times 2016;33(7)):
If a person does not meet these standards, their capacity to consent is most likely impaired. But capacity to consent to sexual activity is on a continuum. An individual may have the capacity to consent to activities with a low level of risk, like cuddling and kissing, but not intercourse, which carries a higher level of risk (Syme ML and Steele D, Arch Clin Neuropsychol 2016;31(6):495–505).
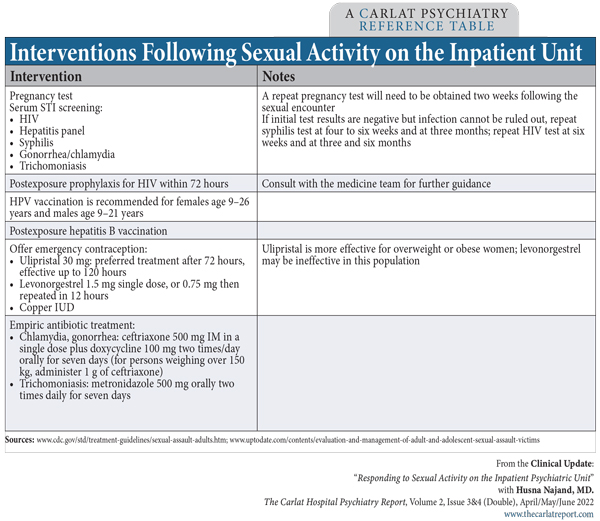
If both patients report the sexual activity was consensual and both have the capacity to consent to sexual activity, do you need to intervene any further? Generally not. The exception is if there was sexual intercourse, in which case you should inform the patients of the risks of unprotected sex and offer screening and prophylactic interventions (see “Interventions Following Sexual Activity on the Inpatient Unit” table below).
Guidelines for managing non-consensual sexual incidents
What do you do if the patients claim the activity was consensual but one or both lack the capacity to consent to sexual activity? The surrogate decision maker for the patient(s) lacking capacity must be contacted immediately to determine the steps they wish to take. State regulations generally require you to report such incidents to a department of public health or department of mental health. The reporting follows the same procedures used for any so-called “serious reportable event,” such as self-inflicted or physical assaults. Reach out to your hospital’s risk management team with any questions.
If a patient reports the activity was not consensual, this constitutes sexual assault. Ensure the patient is safe and is kept separated from the alleged perpetrator. If the patient wants to press charges, contact the police and arrange for a private meeting. Depending on the nature of the contact, a rape kit should be offered, which is handled by a hospital’s sexual assault response team. If your hospital does not have such a service, the patient may be transferred briefly to another hospital. Offer the patient counseling, given the psychological impacts such activity may have (counseling can also help even in cases where the sexual activity was consensual). Watch for unconscious biases: We might tend to view a petite female patient as a victim and a large male patient as a perpetrator, but all patients on inpatient units are vulnerable adults, and we need to follow the same procedures for all cases.
Keep in mind that patients have the right to refuse the recommended examinations and interventions unless they lack capacity to make informed decisions. In those cases, identify a surrogate decision maker who can make decisions on the patient’s behalf.
Document all details of the incident, clinical evaluations, and interventions in the medical record. Include information on the location, timing, individuals involved, witnesses, clinical evaluations (including for capacity), interventions offered and completed, follow-ups, and referrals. Finally, debrief with the team to review staff response and management of the incident, with the goals of minimizing future incidents and maintaining patient safety.
CHPR Verdict: When a sexual incident occurs on the inpatient psychiatric unit, assess each patient privately to determine if the incident was consensual and if they each had the capacity to consent to sexual activity. Work with your hospital’s risk management team to make sure all appropriate authorities are notified and to assist with next steps. Notify the police if the patient wants to press charges. Follow clinical guidelines regarding physical examinations, laboratory testing, and prophylactic treatment.
Hospital PsychiatryHospital policies regarding physical contact
Many psychiatric hospitals lack specific policies on patient-to-patient physical contact. Perhaps these policies are absent because hospital administrators view such contact as obviously inappropriate, for a variety of reasons. Sexual contact elicits strong emotions, both positive and negative, that may distract from or interfere with treatment. If sexual contact is non-consensual or involves patients with reduced capacity, it can be both criminal and psychologically damaging.
What about more casual physical contact, such as holding hands, sitting very close to others, or hugging? Patients often make intense connections with others in inpatient units, given the encouragement to be honest and self-revealing in treatment groups. Touching may seem like a natural extension of emotional intimacy. Nonetheless, there is a slippery slope from friendly touching to sex, so most units err on the side of caution and completely prohibit physical contact between patients. Generally, we agree that such policies are prudent. We remind patients of these policies at the beginning of and during the course of their inpatient stays, particularly when they display hypersexual behaviors.
How to respond to sexual contact in the hospital
The nursing or security staff inform you that two patients on the unit have engaged in sexual activity. What do you do next? First, determine what type of sexual activity occurred. In most cases on inpatient units, sexual activity occurs between fully clothed individuals and involves kissing, hugging, and fondling. Actual sexual intercourse is rare. You will generally have a good idea of what happened from the reports of the unit staff who discovered the activity, but you should do your best to confirm this when you interview the patients yourself. Separate the patients and place them under 1:1 supervision while you evaluate each privately. Patients should not change clothing or take showers during this time, as physical evidence may be needed. Be sure to inform the hospital’s risk management office of the incident.
Determine capacity to consent
Regardless of the nature of the activity, you should try to determine whether the patients had the capacity to consent to sexual activity. All individuals—including those with severe mental illness, as well as those with intellectual disabilities or dementia—have sexual consent capacity once they reach the age of consent as established by their state. Patients on psychiatric holds also retain sexual consent capacity; the exception is if a court previously determined a patient lacks capacity, such as in probate conservatorship. Assuming the patients involved are their own decision makers, how do you determine if they really have the capacity to consent to sexual activity? While each state has its own statutes, the following principles have typically been used to determine sexual consent capacity (Boni-Saenz AA, Psychiatric Times 2016;33(7)):
- Knowledge: Does the patient demonstrate basic knowledge and understanding of the sexual act in question?
- Rationality: Does the patient demonstrate reasoning ability, including weighing the risks and benefits of sexual activity and appreciating its potential consequences (eg, STI transmission, pregnancy)?
- Voluntariness: Is the patient able to decide to engage in sexual activity without coercion or undue influence? Does the patient understand they have the right to say no (withdraw consent) at any time during the sexual activity?
If a person does not meet these standards, their capacity to consent is most likely impaired. But capacity to consent to sexual activity is on a continuum. An individual may have the capacity to consent to activities with a low level of risk, like cuddling and kissing, but not intercourse, which carries a higher level of risk (Syme ML and Steele D, Arch Clin Neuropsychol 2016;31(6):495–505).
If both patients report the sexual activity was consensual and both have the capacity to consent to sexual activity, do you need to intervene any further? Generally not. The exception is if there was sexual intercourse, in which case you should inform the patients of the risks of unprotected sex and offer screening and prophylactic interventions (see “Interventions Following Sexual Activity on the Inpatient Unit” table below).
Guidelines for managing non-consensual sexual incidents
What do you do if the patients claim the activity was consensual but one or both lack the capacity to consent to sexual activity? The surrogate decision maker for the patient(s) lacking capacity must be contacted immediately to determine the steps they wish to take. State regulations generally require you to report such incidents to a department of public health or department of mental health. The reporting follows the same procedures used for any so-called “serious reportable event,” such as self-inflicted or physical assaults. Reach out to your hospital’s risk management team with any questions.
If a patient reports the activity was not consensual, this constitutes sexual assault. Ensure the patient is safe and is kept separated from the alleged perpetrator. If the patient wants to press charges, contact the police and arrange for a private meeting. Depending on the nature of the contact, a rape kit should be offered, which is handled by a hospital’s sexual assault response team. If your hospital does not have such a service, the patient may be transferred briefly to another hospital. Offer the patient counseling, given the psychological impacts such activity may have (counseling can also help even in cases where the sexual activity was consensual). Watch for unconscious biases: We might tend to view a petite female patient as a victim and a large male patient as a perpetrator, but all patients on inpatient units are vulnerable adults, and we need to follow the same procedures for all cases.
Keep in mind that patients have the right to refuse the recommended examinations and interventions unless they lack capacity to make informed decisions. In those cases, identify a surrogate decision maker who can make decisions on the patient’s behalf.
Document all details of the incident, clinical evaluations, and interventions in the medical record. Include information on the location, timing, individuals involved, witnesses, clinical evaluations (including for capacity), interventions offered and completed, follow-ups, and referrals. Finally, debrief with the team to review staff response and management of the incident, with the goals of minimizing future incidents and maintaining patient safety.
Table: “Interventions Following Sexual Activity on the Inpatient Unit”
(Click to view full-size PDF.)
CHPR Verdict: When a sexual incident occurs on the inpatient psychiatric unit, assess each patient privately to determine if the incident was consensual and if they each had the capacity to consent to sexual activity. Work with your hospital’s risk management team to make sure all appropriate authorities are notified and to assist with next steps. Notify the police if the patient wants to press charges. Follow clinical guidelines regarding physical examinations, laboratory testing, and prophylactic treatment.
KEYWORDS assault capacity consensual consent debriefing hospital-policy hypersexual-behaviors post-exposure-prophylaxis pregnancy-testing reporting-requirements risk_management sexual-intercourse sti-screening
Issue Date: March 23, 2022
Table Of Contents
Recommended
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2026 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



