A Practical Guide to Light Therapy
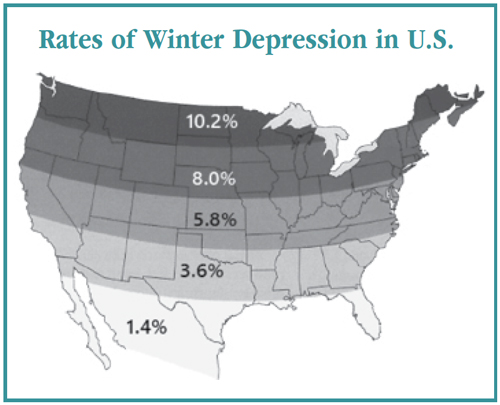
Outdoor living, morning light, evening darkness, and regular rhythms of sleep and waking all have one thing in common: They prevent depression. That’s the conclusion of many large epidemiologic studies, but for people who work indoors and wake up to dark winter mornings, this isn’t good news (Asai Y et al, J Affect Disord 2018;241:235–240). Here’s where light therapy fits in.
Light therapy was discovered at the NIMH in the early 1980s. It has since become a standard treatment for winter depression, with over 100 clinical trials and an effect size that compares favorably to medication: 0.5–0.8 (Mårtensson B et al, J Affect Disord 2015;182:1–7). It also works in non-seasonal depression, possibly because indoor living affords limited access to bright light. Even the brightest indoor spaces (500 lux) are only half as bright as an overcast day (1,000 lux) and far darker than a sunny one (10,000–30,000 lux).
Other photosensitive disorders that show promise with light therapy include ADHD, bulimia, dementia, Parkinson’s disease, and sexual dysfunction in men, as well as circadian rhythm disorders such as shift work, jet lag, and insomnia due to delayed sleep phase disorder (aka extreme night owls) (Botanov Y and Ilardi SS, PLoS One 2013;8:e75893).
To use this therapy, you’ll need to know a few basics, starting with how to recommend the right device.
Selecting a light box
The more popular a light box is, the less likely it is to work. That’s because the qualities that make a light box commercially attractive—slimness, portability, and unobtrusiveness—will also keep it from giving off enough light to treat depression. Here’s what is required: a large screen (at least 12 x 17 inches) that hangs over the head and gives off intense light (at least 2,000 lux; 10,000 lux is ideal) in the white spectrum. “Full spectrum” and blue lamps do not have good evidence for better efficacy, but they do cause problematic glare.
To simplify this process, a group of researchers has stepped in with specific product recommendations at www.cet.org. Currently they recommend Northern Light Technology’s BOXelite OS ($180). Another good option that has been used in clinical trials is Carex’s Day-Light Classic or Classic Plus ($100–$140; the regular Classic has folding stands). The bulbs on a light box will lose a little of their therapeutic intensity over time, even if they continue to appear bright, so they work best when replaced every 2–3 years. Replacement bulbs are around $20 on Amazon (BOXelite uses Philips PL-L 36W or Sylvania FT36DL; Carex uses DL930 bulbs).
Timing the treatment
It’s not just the quantity of light, but the timing that matters. Light therapy works in part by setting the biological clock, and morning light has the most potent effect on that circadian system. The “sweet spot” for light therapy is generally between 5:00 a.m. and 8:00 a.m. and depends on whether the patient is a morning person (closer to 5:00 a.m. is ideal) or a night owl (closer to 8:00 a.m. is ideal). Michael Terman’s group at Columbia University developed a self-report scale to predict the optimal start time (the Morningness-Eveningness Questionnaire or AutoMEQ at www.cet.org/assessment/confidential-self-assessments).
Most patients with depression need 30–60 minutes of light therapy per day; mild cases may need as little as 15 minutes. Patients should start to see improvement within 1–2 weeks. If they have not recovered after 4 weeks, try to increase the duration (eg, up to 2 hours). Patients with a strong seasonal pattern should start the therapy preventatively 2 weeks before their winter episodes typically begin. Light therapy can also augment antidepressants, both in seasonal and non-seasonal depression, with an effect size that compares well to other augmentation strategies (0.5) (Penders TM et al, Prim Care Companion CNS Disord 2016;18(5). doi: 10.4088/PCC.15r01906).
Positioning the box
Patients should sit with the box slightly tilted at a 30° angle over their head. They can read, eat, use a computer, or meditate under the light, but should avoid looking directly into it for the same reasons they shouldn’t stare at the sun. They can wear glasses as long as they don’t have transition, blue light–blocking, or tinted lenses. The intensity of the light falls exponentially with distance, so their head should stay 10–14 inches from the screen, depending on the light box model.
Troubleshooting
Many patients are skeptical of light therapy. I’ll emphasize that it’s as effective as an antidepressant and alters neurotransmitters like serotonin, dopamine, and melatonin. Others accept that light is beneficial, but think that a sunroom or bright reading lamp will suffice. All of those are helpful, but they emit an intensity of light that was used as a placebo in the light therapy trials (300–1,000 lux). On the other hand, morning aerobics or a 1-hour outdoor walk in the winter has good evidence of effectiveness in seasonal depression.
Timing is another obstacle. If early morning is not practical, patients can still benefit by using the light box later in the day, as long as it’s not past 2:00 p.m. After that time, light therapy will actually flip the biological clock in the wrong direction, possibly resulting in depression, insomnia, and mania. Patients who have difficulty getting out of bed to start light therapy can benefit from a dawn simulator, which improves wakefulness and energy in the morning (see TCPR, February 2019).
Safety
Light therapy is well tolerated. Headaches, eye strain, and mild nausea are the most common adverse effects. The main risk is the exposure to high-intensity light, which can damage the skin and eyes. Recommended boxes have a diffusion screen that filters out ultraviolet light, the most harmful ray. Blue light, which lies next to the ultraviolet spectrum, will still pass through and may pose a problem for patients who have retinal disease or take photosensitizing medications like lamotrigine, antipsychotics, or tricyclics. Reports of actual problems are very rare, but patients should consult with their ophthalmologist if this is a concern (Brouwer A et al, Acta Psychiatr Scand 2017;136:534–548).
TCPR Verdict: Light therapy is a top recommendation for seasonal depression and can work in non-seasonal and bipolar depressions as well. It’s an investment of time (30–60 minutes a day), but it causes few side effects and has benefits that compare favorably to those of antidepressants.
Light Therapy in Bipolar Disorder
Winter depression is common in bipolar disorder, but in spring the sudden increase in sunlight can cause mania and mixed states. Likewise, case reports suggest that light therapy can trigger mania, especially if it’s titrated too quickly or delivered in the early morning. Manic symptoms are less likely with midday treatment (12:00–2:00 p.m.), and this strategy worked well in a randomized controlled trial in non-seasonal bipolar depression. The light was titrated slowly, starting with 15 minutes a day and increasing by 15 minutes each week toward a target of 1 hour (Sit DK et al, Am J Psychiatry 2018;175:131–139).
If midday treatment is impractical, morning light might be safe in bipolar. It worked well without manic induction in 2 controlled trials, and in a literature review, it was not associated with manic switching in 799 patients with bipolar disorder (Benedetti F, Psychiatry Res 2018;261:351–356). However, I’d stick with the midday protocol if the patient has bipolar I disorder or a recent problem with manic or mixed symptoms (in bipolar terms, recent means the past 6 months). If mixed symptoms emerge during light therapy, decrease the time under the light box, move it to midday, or stop the treatment entirely. Or, you could try dark therapy.
Dark therapy is the corollary of light therapy. It has mood-stabilizing effects and can be used in the evenings after morning light therapy to prevent mania. Dark therapy requires patients to stay in pitch darkness or wear blue light–blocking glasses from early evening (around 6:00 or 8:00 p.m.) to morning (8:00 a.m.) (see TCPR, February 2019). Again, timing is the issue with light and darkness. Dark mornings can cause depression, but darkness at night improves depression and mania based on large epidemiologic and small clinical trials (Obayashi K et al, Am J Epidemiol 2018;187(3):427–434).
Newsletters
Please see our Terms and Conditions, Privacy Policy, Subscription Agreement, Use of Cookies, and Hardware/Software Requirements to view our website.
© 2026 Carlat Publishing, LLC and Affiliates, All Rights Reserved.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



