Managing Insomnia in Older Adults
Mr. Johnson is a 74-year-old man with depression, hypertension, and obesity. He presents to your clinic complaining of trouble falling asleep. He has tried trazodone in the past to poor effect. What do you do next?
Over 50% of older adults (OAs) report sleep difficulties (Patel D et al, J Clin Sleep Med 2018;14(6):1017–1024). Specific criteria for insomnia vary, but all include subjective discontent with sleep quality or quantity, with one or both of the following: difficulty initiating sleep (sleep-onset insomnia) or frequent awakenings and/or early-morning awakenings (sleep-maintenance insomnia).
Durational definitions of insomnia include:
- Episodic insomnia: lasting at least one month but less than three months
- Persistent insomnia: occurring at least three nights per week for longer than three months
- Recurrent insomnia: two or more episodes in one year
Although the incidence of insomnia increases with age, it is not a normal part of aging. Normal sleep changes in OAs include:
- Decreased total sleep needs
- Decreased slow-wave and REM sleep
- Advanced sleep phase (eg, falling asleep earlier and waking up earlier)
(Source: Hirshkowitz M et al, Sleep Health 2015;1(1):40–43)
Evaluation
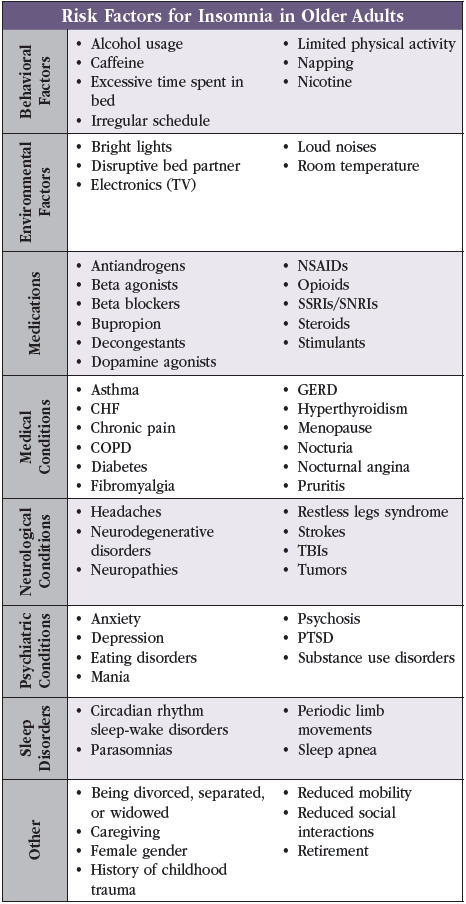
Insomnia is a clinical diagnosis, so taking a good history is the first step. Knowing basic risk factors for insomnia (eg, alcohol use, overnight disruptions, poor sleep hygiene, certain medications) and understanding that insomnia can be a primary disorder or comorbid condition can help guide questions (see “Risk Factors for Insomnia in Older Adults” table).
Diagnostic tools
Additional diagnostic tools include brief screens such as the:
- Geriatric Depression Scale (GDS) for depression
- Generalized Anxiety Disorder 7 (GAD7) for anxiety
- Insomnia Severity Index (ISI) and the more detailed Pittsburgh Sleep Quality Index (PSQI) for sleep problems
Most evaluations for insomnia also include a patient-recorded sleep diary (minimum two weeks) to clarify patterns of going to bed and waking up, number of awakenings, and total time spent in bed. Sometimes a sleep diary can show that a patient’s sleep parameters are appropriate for their age. These patients do not need treatment beyond education and reassurance that it is normal to occasionally sleep poorly.
Additional testing
Only order a polysomnography if you think the patient might have comorbid sleep apnea or parasomnias. While consumer devices for wrist actigraphy, such as smart watches, can compare overall sleep before and after treatment, their accuracy on specific metrics is usually poor. They can also heighten anxiety in patients by putting a focus on their numbers. No specific imaging is needed for the diagnosis either (Patel et al, 2018).
Mr. Johnson scores in the moderate range on both the GDS and GAD7. You ask him to start a sleep journal. During a follow-up, you note that he spends up to 12 hours in bed, with around five awakenings nightly. He identifies a lack of daytime structure and excessive napping as contributing to his poor sleep. You suggest tweaks to his nightly routine, such as going to bed later and replacing TV with reading before bed. You also suggest he download the CBT-I Coach mobile application.
Nonpharmacologic treatment
Sleep hygiene
With any sleep complaints, first address comorbid medical or psychiatric conditions. Then provide counseling on sleep hygiene principles:
- Maintain regular bed and wake times
- Exercise regularly
- Minimize external disruptions
- Eliminate caffeine after lunch
- Decrease nighttime nicotine and alcohol intake
- Reduce napping and time spent in bed outside of sleep and sex
Therapy
After these steps, the first-line treatment for chronic insomnia is cognitive behavioral therapy for insomnia (CBT-I). Compared to medications, CBT-I has longer-lasting effects on sleep and limited side effects (Mitchell MD et al, BMC Family Pract 2012;13:40). However, it can be difficult to find both CBT-I clinicians and patients willing to complete the CBT-I recommendations. Another option is the Brief Behavioral Treatment for Chronic Insomnia (BBTI), which requires fewer sessions and is available in some PCP offices (Buysse DJ et al, Arch Intern Med 2011;171(10):887–895). Motivated patients with smartphones can try the free CBT-I Coach app or the moderately priced, FDA-cleared Somryst app.
Despite a couple weeks of restricting his time in bed, Mr. Johnson still struggles with significant fatigue and anxiety. He tells you his mood is even more depressed. You discuss medication options.
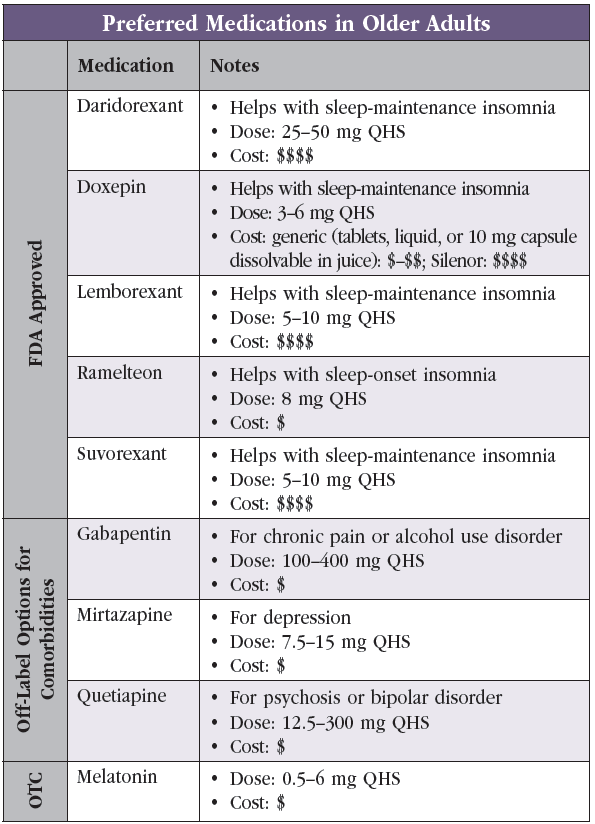
Despite nonpharmacologic efforts, some patients may need medications for insomnia. The goal is for short-term usage only. FDA-approved medications for insomnia include:
- Ramelteon (a melatonin receptor agonist)
- Doxepin (a histamine receptor antagonist)
- Daridorexant, lemborexant, and suvorexant (dual orexin receptor antagonists (DORAs))
- Benzodiazepine receptor agonists (includes nonbenzodiazepines such as eszopiclone, zolpidem, and zaleplon)
Choosing a medication for insomnia
For OAs, avoid benzodiazepine receptor agonists given their potential side effects (eg, increased falls, confusion, daytime sedation, dependence). Note also that benzodiazepines disrupt sleep architecture by further decreasing both slow-wave and REM sleep. See CGPR April/May/June 2022 for more.
Beyond this general recommendation, the choice of medication is highly individualized (Sateia MJ et al, J Clin Sleep Med 2017;13(2):307). Factors include:
- Type of insomnia
- Medication price
- Prior medication trials
- Comorbidities
See “Preferred Medications in Older Adults” table for more.
Comorbidities
Patients presenting for a mental health condition often also report insomnia. In these patients, it is common to use off-label medications to treat multiple symptoms at once:
- Mirtazapine: can help patients with depression and insomnia, but may lead to weight gain (sometimes a desirable side effect).
- Trazodone and amitriptyline: also used for insomnia; not effective for the treatment of depression at doses used for sleep.
- Gabapentin: taken at night; benefits patients with chronic pain, restless legs syndrome, or alcohol use disorder and insomnia.
- Sedating antipsychotics (eg, quetiapine): for patients with a primary psychotic disorder or bipolar disorder to help with sleep. Risks do not outweigh the benefits for use as a sleep aid for nonpsychotic patients!
Over-the-counter options
There are also many over-the-counter (OTC) sleep aids and dietary supplements patients might ask about:
- Diphenhydramine and doxylamine: not recommended for OAs due to anticholinergic properties. Some research suggests anticholinergics can increase dementia risk (Coupland C et al, JAMA Intern Med 2019;179(8):1084–1093).
- Melatonin: well tolerated when taken a few hours before bedtime; can help slightly shorten sleep onset.
- Other OTC options: not enough research to confidently give patients other recommendations.
After joining a gym, starting ramelteon 8 mg oral nightly for one month, and implementing basic CBT-I principles, Mr. Johnson sees a 20-minute improvement in sleep onset in his sleep diary.
CARLAT VERDICT
Addressing comorbidities and reducing risk factors is a good first step in improving sleep. CBT-I is the first-line treatment for insomnia in OAs. Try to avoid benzodiazepine receptor agonists. If a patient needs a short-term medication, then DORAs, ramelteon, and doxepin are FDA approved for insomnia. For patients who may have difficulty affording newer medications, use generic doxepin or ramelteon. Melatonin is also a safe and affordable alternative.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



