Addressing Polypharmacy in Older Adults
Ms. Andrews is 87 years old with stage 4 bladder cancer and recent visual hallucinations. She has just completed a course of ciprofloxacin for a presumed urinary tract infection (UTI). She has taken amitriptyline 50 mg for many years to manage neuropathic pain and relies on over-the-counter (OTC) ibuprofen PM for insomnia. Her PCP initiates quetiapine 50 mg QHS to address her hallucinations and refers her to you for further evaluation.
We know polypharmacy poses risks for older adults (OAs), including side effects, drug interactions, and decreased medication adherence. In this case-based article, we offer tips for preventing these problems and ensuring your prescribing decisions make sense.
Confirm the diagnosis
In our case vignette, the patient was prescribed quetiapine for presumed visual hallucinations—which is reasonable at first glance. But good prescribing means taking time to confirm your diagnosis, especially when contemplating risky medications like an antipsychotic.
Your psychiatric evaluation reveals that Ms. Andrews has no history of psychosis and has only experienced visual hallucinations after taking “strong pain medications” following a hip fracture. Her daughter tells you she has no history of dementia and her memory seemed fine before her recent UTI. You notice she occasionally struggles to find the right words, displays variable attention, and demonstrates small gaps in her recent memory. Given the recent onset of this cognitive impairment, you diagnose her with delirium.
Cognitive complaints always call for a review of the history:
- Has the impairment been documented in the past?
- Has there been a gradual decline consistent with major neurocognitive disorder, or has the decline been abrupt?
- Is there a connection between recent medical issues and psychiatric symptoms?
- Have you spent enough time interviewing informants such as family members or past caregivers?
Reconsider medication and dose
According to her daughter, Ms. Andrews has taken quetiapine 50 mg nightly for the last five days. On interview, the patient is sedated and tremulous. Her daughter says she has been less steady on her feet.
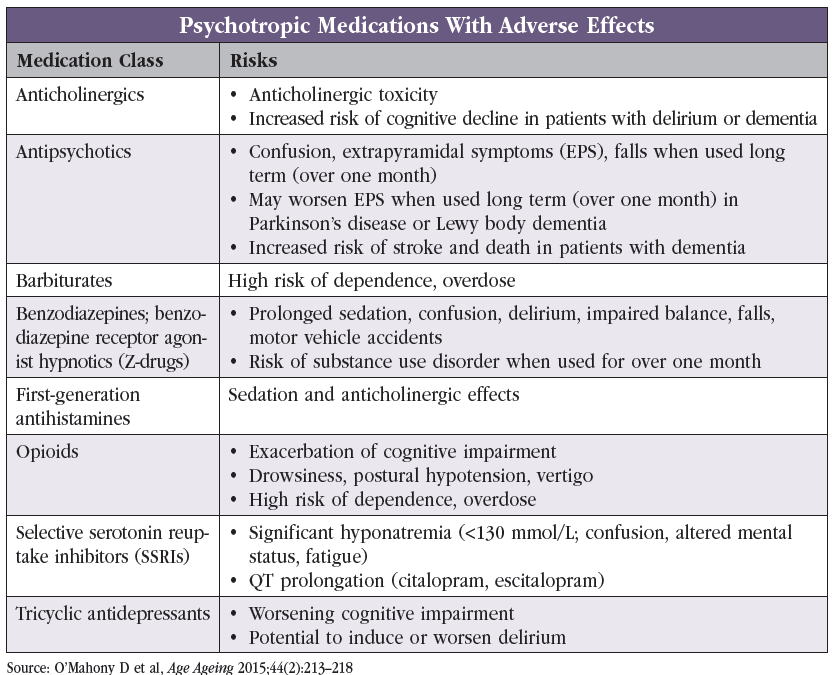
When finding the right medication for OAs, take the patient’s medical history and comorbidities into account and try to prevent potential drug interactions. See “Psychotropic Medications With Adverse Effects” table.
Determining the right dose is especially important in OAs, who may be more sensitive to medications due to age-related physiological changes:
- Aging affects medication distribution due to changes in muscle mass and body fat
- Decreases in hepatic and renal function slow the elimination of medications
In this patient’s case, a too-high dose of quetiapine resulted in unsteadiness, tremulousness, and sedation. She may have tolerated quetiapine better at a lower dose, such as 12.5 mg.
Evaluate treatment response
We often become impatient when a patient’s symptoms are not improving. But it’s important to wait for a drug to take effect to know whether the patient responds to it. Before increasing dosage or adding new medications, confirm that the patient takes the medication as prescribed. If adherence is not an issue, educate patients on the time it takes for their medication to work.
Employ shared decision making
Shared decision making prioritizes the patient’s treatment goals and preferences. Before changing medications, consider asking the patient:
- What matters to them? Are they more interested in avoiding side effects, or are they willing to tolerate side effects to achieve full symptom resolution?
- Are they prepared to manage one more medication?
- Can they participate in necessary monitoring (eg, attending appointments and obtaining labs)?
Use these discussions to educate patients about the risks of polypharmacy and as a starting point to reduce their medications.
Identify key medications
Among a patient’s medication list, a few probably stand out as essential. Prioritize these medications and try to reduce anything that could harm the patient. The two sets of criteria from the American Geriatrics Society and the British Geriatrics Society—Beers and STOPP criteria, respectively—can help identify these potentially inappropriate medications (2023 American Geriatrics Society Beers Criteria Update Expert Panel, J Am Geriatr Soc 2023;71(7):2052–2081; O’Mahony D et al, Age Ageing 2015;44(2):213–218).
OTC medications
Often overlooked, OTC medications can significantly impact a patient’s medication profile. Review commonly used OTC medications like antihistamines (in cold and flu products, antiemetics, and sleep preparations), proton pump inhibitors, and nonsteroidal anti-inflammatory drugs with every patient. Pay attention to “PM” sleeping aids, which often contain anticholinergic activity.
Acknowledge patient vulnerabilities
Identify each patient’s vulnerabilities to guide discussions about potential side effects. Ask about past adverse medication experiences, considering:
- Frailty
- Cognitive impairment
- Appetite changes
Simplify medication regime
Try to use medications that address multiple symptoms at once. Look for regimens that require fewer daily doses to minimize the pill burden (eg, using extended-release drug formulations).
Ms. Andrews’ hallucinations resolve after she finishes the ciprofloxacin course. You explain that her nighttime medications (especially ibuprofen PM, which contains diphenhydramine) may have increased her risk for delirium. After learning that her OTC medication can affect her cognition, she decides to discontinue it.
 Monitor for adverse events and prescribing cascades
Monitor for adverse events and prescribing cascades
This patient’s use of ibuprofen PM could have gone under the radar for a long time. As clinicians, we should proactively ask about symptoms that patients might not report, such as changes in memory, urinary incontinence, and orthostasis.
Think of new symptoms as medication related until proven otherwise and remain vigilant for prescribing cascades—when one drug leads to another due to side effects, creating a domino effect of prescriptions (Rochon P and Gurwitz J, Lancet 2017;389(10081):1778–1780). Example cascades include:
- Prescribing medications for urinary incontinence after starting a cholinesterase inhibitor
- Starting antihypertensives after prescribing stimulants or venlafaxine
- Adding medications for nausea or constipation after starting a selective serotonin reuptake inhibitor
Ms. Andrews discontinues quetiapine after you determine that her hallucinations were likely secondary to her UTI. She is agreeable to a trial of lowering her amitriptyline dose to 25 mg QHS after you explain the physiologic effects of aging on drug metabolism.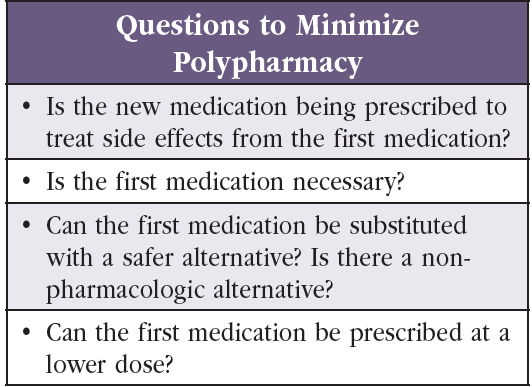
Specific medication classes
Although many psychiatric medications increase fall risk and affect cognition in OAs, a few stand out:
- Benzodiazepines and benzodiazepine receptor agonists (eg, zolpidem and zopiclone)
- Certain antidepressants and mood stabilizers
- Antipsychotics
- Strong anticholinergic medications
For more information, visit www.thecarlatreport.com/highriskmedsolderadults and www.thecarlatreport.com/anticholinergicactivity.
Sedatives, anxiolytics, lithium, and antipsychotics significantly increase emergency department (ED) visits compared to other psychiatric medications. Zolpidem has been implicated in adverse drug event–related ED visits more frequently than any other psychiatric medication, especially among OAs (Hampton LM et al, JAMA Psychiatry 2014;71(9):1006–1014).
When using sleep aids, peel back these medications first and encourage consideration of other treatments, including good sleep hygiene and relaxation techniques. If behavioral interventions aren’t enough, consider switching to a medication with fewer risks (eg, melatonin or ramelteon).
End-of-life care considerations
Goals of care discussions often prompt reconsideration of a patient’s medications:
- Discontinue medications when the benefits materialize after weeks or months, possibly exceeding a patient’s life expectancy.
- Shift focus to maximize quality of life. Reach for high-risk medications, such as opioids, sedatives, and anticholinergics, to make the patient comfortable (for more on end-of-life care, see CGPR Oct/Nov/Dec 2023).
CARLAT VERDICT
Address polypharmacy, especially after hospitalization, transitions of care, and when multiple clinicians are involved. Engage patients and their families in shared decision-making to ensure optimal prescribing.


_-The-Breakthrough-Antipsychotic-That-Could-Change-Everything.webp?t=1729528747)



